Contents
What is Aspirin
- Aspirin is a prototypical analgesic, fibrinolytic and anti-inflammatory drug which is used for the treatment of fever, inflammation and mild to moderate pain.
Aspirin generic and brands name
- The drug is available under generic name Acetylsalicylic acid (ASA) and brand name
- Active component of aspirin i.e. salicylic acid was initially isolated by Edward Stone from the bark of willow tree in 1763.
- Aspirin was first synthesised by Felix Hoffmann at Bayer in
- Aspirin is manufactured and marketed by pharmaceutical company Bayer Health Care.
- Aspirin is also manufactured by Merck Pharmaceuticals under brand name Acetophen.
What is the source of the drug (natural or synthetic)
- Aspirin is a synthetic (man-made) pharmaceutical non-steroidal anti-inflammatory
What is the use of aspirin
- Aspirin plays a key role in the treatment of inflammatory diseases such as rheumatoid arthritis (a progressive autoimmune disease primarily causes inflammation in joints) and osteoarthritis (a disease of joint caused by breakdown of joint cartilage).
- Usually, Aspirin is used in the treatment of Fever and mild to moderate Pain due to headache, arthritis, menstrual periods and muscle aches.
- It is also used in the treatment of Systemic lupus erythematosus (autoimmune disease of connective tissues) and other rheumatologic conditions.
- Aspirin is also prescribed for patients of heart attack to reduce the risk of heart attack and deaths caused by heart attack.
- Aspirin is usually recommended for the patients of ischemic stroke (blockage of blood flow to brain due to blood clot) or mini stroke (blockage of blood flow to brain for short time).
- This drug is also used to treat the angina (sensation of chest pain occur when heart muscle does not get enough oxygen).
- However, Aspirin does not used to prevent the hemorrhagic strokes (leakage of blood around the brain due to the rupture of blood vessel).
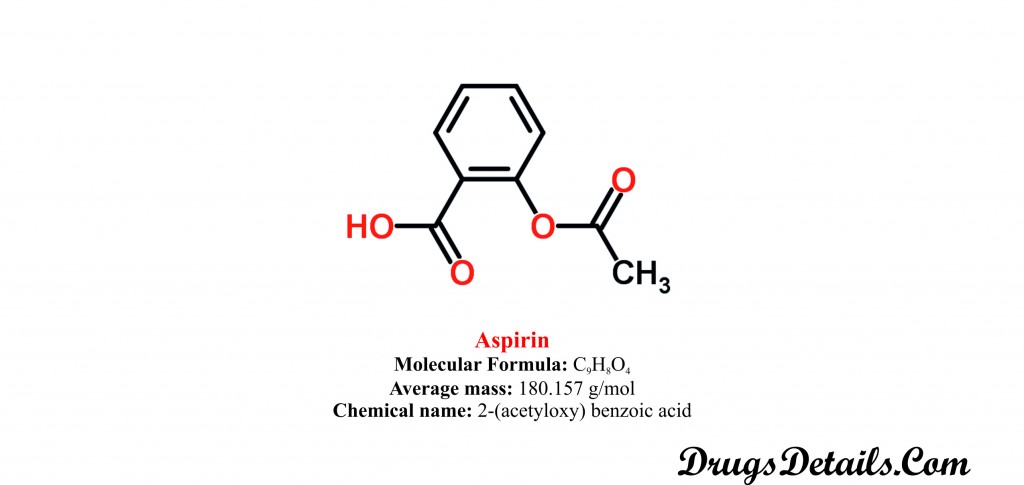
Pharmacophore structure: Information about the chemical structure of the drug
Aspirin chemically belongs to the class of organic compounds which are known as phenol esters characterized by benzene ring substituted by a hydroxyl group and an ester group. The detailed chemical classification of Aspirin is described below:
| Kingdom | Organic compounds |
| Super Class | Benzenoids |
| Class | Benzene and substituted derivatives |
| Sub Class | Phenol esters |
| Direct Parent | Phenol esters |
Chemical information of the drug
- Aspirin is available as acetylsalicylic acid and acts by inhibiting the synthesis and release of prostaglandins.
- It is a synthetic pharmaceutical Aromatic homomonocyclic compounds with a molecular formula C9H8O4.
- The molecular weight of the Aspirin is 157 g/mol.
- Chemically, Aspirin is known as 2-(acetyloxy) benzoic acid.
- Aspirin is odourless, white, granular or needle-like crystalline powder and has water solubility of 46 mg/mL.
- Aspirin is freely soluble in alcohol, sparingly soluble in absolute ether, soluble in chloroform and ether and slightly soluble in water. Aspirin is highly lipid soluble.
- The melting point of Aspirin is 135°C while the boiling point of Aspirin is 140°
- Aspirin is available in the form of regular strength tablets and caplets, extra strength tablet, delayed-release tablet and quick chewable tablets for oral administration with food or without food.
- ASPIRIN regular strength tablets are available in strength of 325 mg.
- It is round in shape and white in color crossed with BAYER on both side.
- Aspirin regular strength tablets contain acetylsalicylic as active component and powdered cellulose, corn starch, hypromellose and triacetin as inactive constituent.
- ASPIRIN regular strength caplets are available in strength of 325 mg.
- It is capsule shaped, white in color scored on one side and crossed with BAYER on other side.
- Aspirin regular strength caplets contain acetylsalicylic as active component and powdered cellulose, corn starch, hypromellose and triacetin as inactive constituent.
- ASPIRIN extra strength tablets are available in strength of 500 mg.
- It is round in shape, white in color crossed with BAYER on one side in red ink.
- Aspirin extra strength tablets contain acetylsalicylic as active component and powdered cellulose, corn starch, hypromellose carnauba wax, shellac, propylene glycol, titanium dioxide, triacetin, D&C Red No. 7, FD&C Blue No. 2 and FD&C Red No. 40 as inactive constituent.
- ASPIRIN delayed release tablets are available in strength of 81 mg.
- It is pale blue in color, enteric coated and marked with 81 on one side.
- Aspirin delayed release tablets contain acetylsalicylic as active component and powdered cellulose, corn starch, hypromellose carnauba wax, croscarmellose sodium, lactose monohydrate, methacrylic acid polymer, microcrystalline cellulose, polysorbate 80, sodium lauryl sulphate, starch, shellac, propylene glycol, titanium dioxide, triacetin, FD&C Blue No. 1 and FD&C Blue No. 2 as inactive constituent.
- ASPIRIN quick chew tablets are available in strength of 81 mg.
- It is peach colored with pleasant orange taste and crossed with BAYER on one side.
- Aspirin quick chew tablets contain acetylsalicylic as active component and dextrose, corn starch, sodium cyclamate, orange juice flavour and FD&C Yellow No. 6 as inactive constituent.
- ASPIRIN regular strength tablets are available in strength of 325 mg.
Aspirin mechanism of action
How the medicine works (mode of action)?
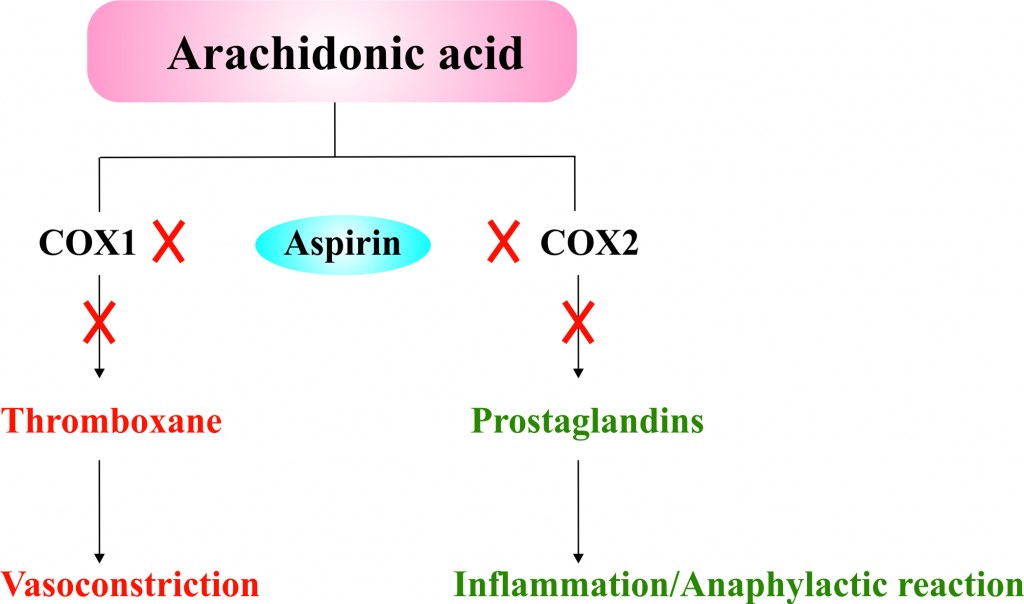
- Aspirin is a non-steroidal anti-inflammatory drug that inhibits cyclooxygenase (COX) enzyme therefore known as COX inhibitor agent.
- Cyclioxygenase enzyme (namely COX1 and COX 2) known as prostaglandin-endoperoxide synthase (PTGS), that coverts arachidonic acid in to prostanoids, including thromboxane (mediators of vasoconstriction) and prostaglandins (mediators of inflammatory and anaphylactic reactions).
- The action of both acetyl and salicylate component of the acetylsalicylic acid (ASA or Aspirin) and its active metabolite salicylate are liable for the anti-inflammatory and analgesic properties through inhibition of cyclooxygenases.
- ASA inhibits the COX (both COX-1 and COX-2) activity by binding to it irreversibly.
- Inhibition of COX results in reduced formation of precursors of prostaglandins and thromboxane from arachidonic acid.
- Anti-rheumatic or non-steroidal anti-inflammatory effect is caused by the analgesic and anti-inflammatory mechanisms of ASA not by the pituitary-adrenal stimulation.
- Antipyretic effect of ASA is resulted from the intervention in production of Prostaglandin E1 which is a potent pyretic agent.
- ASA also inhibit the aggregation of platelets. This inhibitory effect of ASA is resulted from the intervention in production of Thromboxane A2 which is accountable for the platelets aggregation.
- Acetylsalicylic acid acts as acetyl donor to COX. This acetylation of COX is irreversible and causes the inactivation of the COX. This inactivation results in the prevention of formation of the Thromboxane A2.
Recommended doses of Aspirin
The prescribed dose of Aspirin varies depending upon the age and diseased state of the patient.
- Adult dose:
- Angina Pectoris and Angina Pectoris Prophylaxis: 75 mg to 325 mg in a day orally in single dose.
- Ankylosing Spondylitis: 3 gm in a day in 3 to 4 divided doses orally.
- Fever: 325 mg to 650 mg at interval of 4 hours (maximum 4 gm in a day) orally or by rectal route.
- Ischemic Stroke: 50 mg to 325 mg in a day orally in single dose.
- Myocardial Infarction: 160-162.5 mg in a day orally in single dose.
- Osteoarthritis: 3 gm in a day in 3 to 4 divided doses orally.
- Pain: 325 mg to 650 mg at interval of 4 hours (maximum 4 gm in a day) orally or by rectal route.
- Prophylaxis of Ischemic Stroke: 75 mg to 325 mg in a day orally in single dose.
- Prophylaxis of Myocardial Infarction: 75 mg to 325 mg in a day orally in single dose.
- Prophylaxis of Thromboembolic Stroke: 75 mg to 325 mg in a day orally in single dose.
- Prophylaxis of Revascularization Procedures
- Coronary Artery Bypass Graft: After procedure: 325 mg after 6 hour from beginning the procedure. 325 mg once by oral route daily for a year or until your doctor does not say to stop.
- Percutaneous Transluminal Coronary Angiography
- Before procedure: 325 mg 2 hours prior to procedure.
- After procedure: 160 to 325 mg once by oral route daily until your doctor does not say to stop.
- Carotid Endarterectomy
- Before procedure: 80 mg once a day or may be up to 650 mg twice in a day orally prior to beginning surgery.
- After procedure: 80 mg once a day or may be up to 650 mg twice in a day orally until your doctor does not say to stop.
- Rheumatoid Arthritis: 3 gm in a day in 3 to 4 divided doses orally.
- Rheumatic Fever: 80 mg/kg in a day in 4 divided doses orally (maximum 6.5 gm in a day) for initial 7-14 days and then decrease to 60-70 mg/kg in a day.
- Systemic Lupus Erythematosus: 3 gm in a day in 3 to 4 divided doses orally.
- Paediatric dose:
- Fever: 2 to 11 years: 10 to 15 mg/kg at interval of 4-6 hours orally.
- >11 years: 325 to 650 mg/kg at interval of 4 hours orally.
- Juvenile Rheumatoid Arthritis
- 2 to 11 years (or ≤ 25 kg)
- Initial dose: 60-90 mg/kg in a day in divided doses orally.
- Maintenance dose: 80-100 mg/kg in a day in divided doses orally.
- >11 years (or ≥ 25 kg)
- Initial dose: 2.4-3.6 gm in a day in divided doses orally.
- Maintenance dose: 3.6-5.4 gm in a day in divided doses orally.
- Kawasaki Disease
- Initial dose: 90-130 mg/kg in a day in divided doses orally at interval of 4 to 6 hours for 14 days.
- Maintenance dose: 3-5 mg/kg in a day orally.
- Pain
- 2 to 11 years: 10 to 15 mg/kg at interval of 4-6 hours orally.
- >11 years: 325 to 650 mg/kg at interval of 4 hours orally.
- Rheumatic Fever
- 90-130 mg/kg in a day in divided doses orally at interval of 4 to 6 hours.
- In case of hepatic and renal impairment, the dosing recommendations are as follows:
- Dose in hepatic impairment: The use of Aspirin is case of hepatic impairment is not recommended.
- Dose in renal impairment: In case of chronic renal impairment, caution should be exercised. Not recommended for severe renal impairment.
- Fever: 2 to 11 years: 10 to 15 mg/kg at interval of 4-6 hours orally.
When should I discontinue, withhold or modify the dose of Aspirin
- The usual dosing of the drug may vary depending upon the efficiency and side effects of the drug in a particular individual.
- Do not use the medicine if you are hypersensitive or allergic to any of the ingredients of Aspirin or other analgesic, anti-rheumatic, anti-inflammatory and non-steroidal anti-inflammatory drugs.
- Aspirin is withheld in case of acute gastrointestinal ulcers, severe congestive heart failure, hemorrhagic diathesis and asthma.
- Aspirin is not used for those patients who have coagulation abnormalities such as deficiency of vitamin K and haemophilia.
- Aspirin is also not used in case of deficiency of gluose-6-phosphate dehydrogenase.
- Aspirin is withdrawn in case of hepatic impairment and severe cases of renal impairment.
- However, aspirin is used with carefulness in case of mild to moderate renal impairments.
- Aspirin is contraindicated with the use of other non-steroidal anti-inflammatory drugs such as naproxen (Aleve and Naprosyn), valporic acid (Depakene, Depakote) and phenytoin (Dilantin).
- Use of diclofenac, flurbiprofen, ketoprofen, naproxen and tolmetin with Aspirin is also contraindicated because these drugs can increase the clearance of total drug and decrease the plasma concentration by protein binding displacement.
- Some drugs or chemicals such as benzoic acid, salicylamide, cimetidine and zomepirac may alter or inhibit the metabolism of Aspirin.
- Use of Aspirin with ibuprofen is contraindicated because it may interfere with anti-platelet effect of ASA. Ibuprofen should be taken at least 11 hour after and/or 1 hour previous to the ASA dose.
What are the pharmacokinetic properties of the drug
- Pharmacokinetic studies suggested that after oral administration, Aspirin is absorbed rapidly and completely and has a bio-availability of approximately 80-100%.
- Following absorption the majority (90-99.5%) of the drug is bound to plasma proteins primarily with
- It has been observed that following a 1200 mg dose of maximum (or peak) plasma concentration (17-40mg/l) is achieved in 20-30 minutes in the fasted state.
- The drug is largely metabolized in liver primarily by enzyme
- Acetylsalicylic acid (ASA) largely metabolised into salicyluric acid, ether or gentisic acid and ester or acyl glucuronide.
- The average median half-life of Aspirin is dose dependent. 3.1-3.2 hours for 300-650 mg dose, 5 hours for 1 gm dose and about 9 hours for 2 gm dose.
- Metabolites of Aspirin i.e. salicyluric acid, gentisic acid and acyl glucuronide are mainly excreted in the urine (80-100%). Little amount of metabolites are also excreted through feces and sweat.
- The average steady state volume of distribution of the Aspirin is approximately 5L.
Which pregnancy category (A; B; C; D; X) has been assigned to Aspirin
- The Aspirin is classified by US FDA pregnancy category: N (not classified by FDA).
- Although, aspirin is considered in pregnancy category D.
- There are positive evidences of human fetal risk based on adverse reaction data from investigational and marketing experience or studies in human.
- Aspirin in pregnant women is contraindicated and recommended only when benefit justifies the risk.
- Aspirin may cause increased maternal bleeding during delivery and also affect the cardiovascular system of the foetus.
- Studies support that the aspirin excrete into animal milk as well as in human milk in little quantity. Therefore, breast-feeding is not recommended.
- Despite these facts caution should be exercised when taking Aspirin.
How to take aspirin safely
- Aspirin is available in extended-release tablets and chewable form for oral administration.
- Aspirin tablet is taken by mouth with or without food but in case of gastric upset, it must be taken with food.
- Aspirin extended-release tablets do not chew, split or crush. Whole tablet should be swallowed.
- Chewable tablet should be chewed before swallowing.
- Aspirin tablets must be taken with a glass of water.
- Aspirin tablets should be taken 2 or more times in a day at the intervals of 4 to 6 hours.
- It is also recommended to take drug at almost the same time every day.
- Follow the instructions carefully as directed on prescription leaflet and take Aspirin exactly as directed.
- Do not change the dose of the drug as prescribed by your doctor. Since, the dosage is based on patient medical condition, treatment responses and usage with other drugs.
How to store the drug
- Aspirin is stored at 25°C (77°F) and excursion permitted to 15-30°C (59-86°F).
- Store the medicine away from light and moisture.
- Medicine should not be stored in the bathroom.
- The drug should be kept away from children and pets.
How to properly dispose of expired aspirin
- Throw away unused and opened, outdated or no longer used container.
- Also dispose the old medicine after the expiration date.
- Aspirin should not be dispose in the household garbage, sink or in wastewater.
- Consult your pharmacist or local waste disposal company for proper disposal.
- Aspirin receive its official approval from U.S. Food and Drug Administration (FDA) in June, 1965.
- Aspirin was approved to treat medical complications such as Fever, Pain, Rheumatic Fever, Myocardial Infarction and Ischemic Strokes.
Other uses of the drug
- Aspirin may also be used to treat the rheumatic fever (an inflammatory disease that may cause swelling of the heart valves) and Kawasaki disease (a rare autoimmune disease in children).
- Aspirin may also be used in patients with artificial heart valves to lower the possibility of blood clot.
- Aspirin may also be used for other uses not listed here. It is advisable to ask your doctor or pharmacist for more information.
What special dietary precautions should I follow
- Consult your doctor regarding the use of grapefruit products with your doctor or pharmacist.
- Alcohol consumption can also enhance some side effects of the drug.
What special precautions should I follow/ what should I avoid while using Aspirin
- Before taking Aspirin, tell your doctor about your medical history preferentially if you have any kind of bleeding problems such as haemophilia, liver disease or kidney disease.
- Take advice to your medical health provider if you have ulcers, anaemia, nasal polypus (swelling of nasal lining inside the nasal passage) and asthma.
- Consult with your doctor and pharmacist if you are taking any prescription and non-prescription medications or herbal products.
- Aspirin extended-release tablets should not be used in fever or during pain.
- Alcoholic and alcoholic beverages should be avoided because alcohol increases the level of acetylsalicylic acid about to 50-100% in serum.
- Avoid skipping the dose and do not suddenly stop the medication of Aspirin.
- Stopping the Aspirin medication may enhance the possibility of-
- Blood clots
- Heart attacks
- Strokes and other cardiovascular problems
- Consult your doctor in case of any query.
Aspirin side effects
In addition to the associated benefits, Aspirin also is accompanied with the side effects some of which are common whereas some are more serious. It is always recommended to consult a doctor if you encounter any of the side effects.
Common side effects caused by Aspirin requiring medical attention are as follows:
- Burning in heart
- Nausea
- Stomach pain
- Vomiting
Aspirin may also cause some serious side effects which require immediate medical attention. These include:
- Blood in vomiting
- Bright red blood in stools
- Cold, clammy skin
- Difficulty in breathing
- Fast heartbeat
- Hearing loss
- Hives
- Increased and fast breathing
- Rashes
- Ringing in the ears
- Swelling of the eyes, face, lips, tongue, or throat
- Wheezing
Besides these, Aspirin may also be associated with some other side effects. These include:
- Cardiovascular effects: Hypotension, ventricular ectopy, conduction abnormalities and variant angina.
- Dermatologic effects: Papuloerythroderma, wrinkling in palms and stevens-johnson syndrome.
- Endocrinal effects: Hyperglycaemia and hypoglycaemia in childrens.
- Gastrointestinal effects: Peptic ulcers, esophageal ulceration, hemorrhage, epigastric distress, abdominal pain, gastric mucosal lesions, nausea and vomiting.
- Haematological effects: Megaloblastic anaemia, aplastic anemia, thrombocyturia, thrombocytopenia, hypoprothrombinemia, pancytopenia, eosinophilia and increased blood fibrinolytic activity.
- Hepatic effect: Cholestatic hepatitis and hepatotoxicity.
- Hypersensitivity: Anaphylaxis, rhinitis, urticaria, conjunctivitis, bronchospasm and angioedema.
- Musculoskeletal effects: Rhabdomyolysis.
- Nervous system effects: Confusion, agitation, dizziness, confusion, coma, cerebral edema, cranial hemorrhage, headache, seizures and sometimes hearing loss may occur.
- Ocular effects: Localized periorbital edema.
- Renal effects: Interstitial nephritis, papillary necrosis, renal failure, hematuria, proteinuria, elevation in blood urea nitrogen and creatinine and reduction in glomerular filteration rate particularly in patients with cirrhosis or advanced heart failure.
- Respiratory effects: Pulmonary edema, hyperpnea and tachypnea.
Aspirin overdose
What should I do in case of overdose? If you overdose the drug contact with your doctor or pharmacist for symptomatic and supportive measures. Symptoms of Aspirin overdose may include:
- Cardiovascular failure
- Cerebral edema
- Coma
- Decreased urination
- Dizziness
- Double vision
- Haemorrhage
- Hypotension
- Mental confusion
- Nausea
- Renal failure
- Respiratory alkalosis or failure
- Seizures
- Sweating
- Vomiting
What should I do in case of missed a dose
- Take a missed dose as soon as possible.
- To make up the missed dose, do not take extra medicine.
- Avoid taking the missed dose if it is about time for your next dose.
Aspirin drug interactions
Does Aspirin have any interaction with other drugs? Aspirin may interact with one of the following drugs. Care should be taken when you are taking these medications together.
- Angiogtensin converting enzyme (ACE) inhibitors such as captopril (Capoten), benazepril (Lotensin), perindopril, (Aceon), enalapril (Vasotec), fosinopril (Monopril), lisinopril (Zestril and Prinivil), moexipril (Univasc), quinapril (Accupril), ramipril (Altace), and trandolapril (Mavik). Parallel administration of Aspirin is able to minimize the hypotensive and hyponatremic effect of ACE inhibitors.
- Anticonvulsant drugs such as valpronate or valproic acid (Depakene and Depakote). Concomitant use of Aspirin may cause increase serum level of valpronate.
- Anti-inflammatory drugs such as ibuprofen (Advil, Motrin, Nuprin) and naproxen (Aleve, Naprosyn). Ibuprofen hinder with fibrinolytic effect of Aspirin.
- Anti-inflammatory steroidal hormones such as glucocorticoids which included prednisone, cortisol and betamethasone. Corticosteroides decreases the level of salicylate in the blood through increased salicylate elimination.
- Beta blockers propranolol (Inderal), metoprolol (Lopressor and Toprol XL),nadolol (Corgard), labetalol (Normodyne) and atenolol (Tenormin). Simultaneous administration of aspirin with beta blocker may weaken the hypotensive effect of beta blockers which may result in salt and fluid retention and decline in blood flow.
- Diuretic drugs or water pills such as thiazides (Esidrix and Zaroxolyn), furosemide (Lasix) and bumetanide (Bumex). Use of Aspirin in the company of diuretic drugs decreases the glomerular filtration by means of reduction in prostaglandin synthesis which results in decline sodium excretion.
- Drugs that inhibits the selective serotonin re-uptake (SSRIs) such as citalopram (Celexa and Cipramil), paroxetine (Paxil) and fluoxetine (Prozac and Sarafem). Synergistic effect of SSRIs and Aspirin increased the bleeding in upper gastrointestinal tract.
- Drugs that used as anticoagulant or blood thinners such as heparin and warfarin (Coumadin and Jantoven). Aspirin enhance the anti-coagulant activity of heparin and displace warfarin from binding sites of proteins which increases the possibility of bleeding.
- Inhibitors of carbonic anhydrase enzyme such as acetazolamide (Diamox). Aspirin may increase the serum concentration of acetazolamide.
- Oral hypoglycaemic drugs for example insulin (Humulin and Novolin) and sulfonylurea agents such as chlorpropamide (Diabinese). Aspirin enhance the effect of oral hypoglycaemic drugs which possibly lead to hypoglycaemia.
- Other non-steroidal anti-inflammatory drugs (NSAIDs) such as phenytoin (Dilantin), naproxen (Aleve and Naprosyn). Use of Aspirin with these drugs may decrease renal function and increases bleeding.
- Uricosuric agents such as methotrexate(Trexall), Sulfinpyrazone (Anturane) and probenecid. Aspirin antagonise the action of uricosuric acid.
This list of drugs interacting with Aspirin is not complete and other drugs may also interact with it. Always consult your doctor about the medications you use.
Does Aspirin have any interaction with diseases
It has been observed that following medical conditions (disease) may also interact with Aspirin:
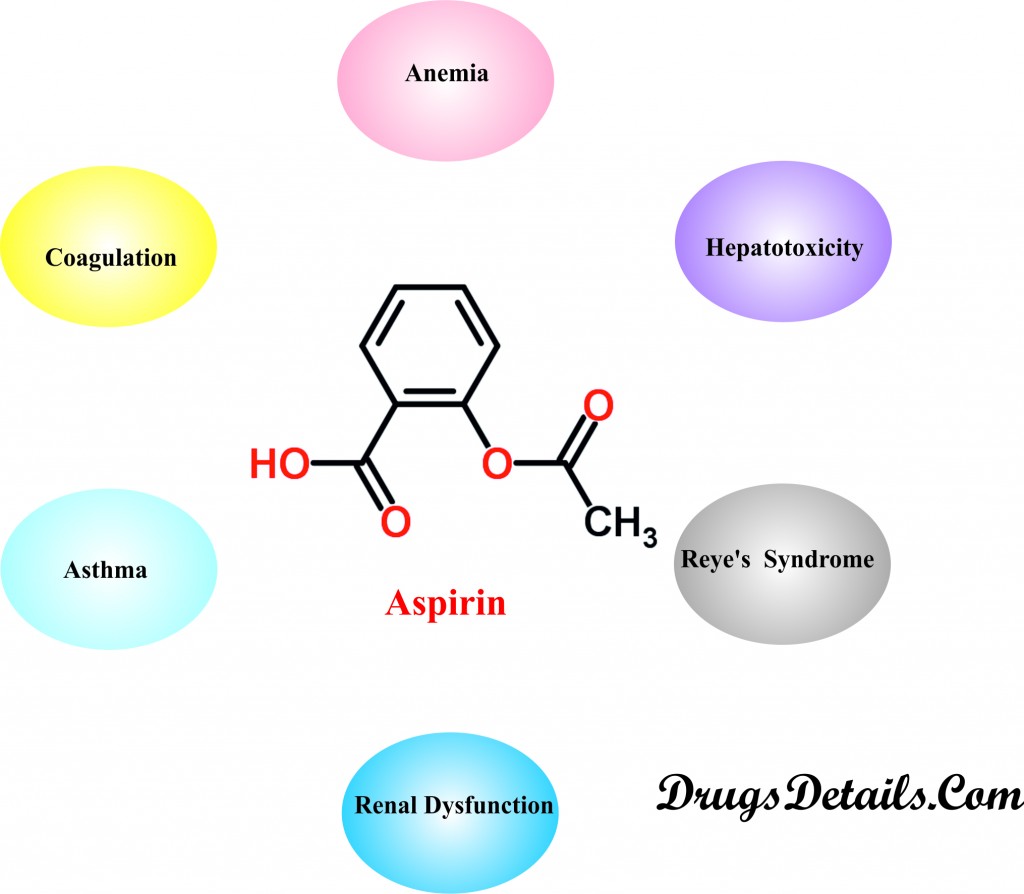
- Coagulation: Aspirin is usually not recommended in patients suffering from bleeding or hemorrhagic disorders including Von Willebrand’s disease, Haemophilia, or Telangiectasia. The drug inhibits platelet aggregation, prolongs bleeding time and hence interferes with coagulation. Administration of Aspirin should be done with extreme caution in patients with vitamin K deficiency, severe hepatic impairment, thrombocytopenia, thrombotic thrombocytopenic purpura, hypoprothrombinemia, or anticoagulant use.
- Anemia: Aspirin usually causes asymptomatic Gastrointestinal (GI) blood loss via its local effect on the GI mucosal membrane which may lead to iron deficiency anemia. Aspirin therapy for an extended period should be done cautiously in patients who are more liable to anemia or suffering from anemia. Periodic monitoring of hematocrit is recommended in such cases.
- Renal Dysfunction: Severe renal impairment demands careful administration of Salicylate drugs including Aspirin and its metabolites as these are eliminated almost entirely by the kidney. Dosage adjustment is required to avoid drug accumulation. Prolonged use may cause renal toxicities (including elevations in serum creatinine, renal papillary necrosis, and acute tubular necrosis) and sometimes renal failure. Aspirin may cause reversible and occasionally a marked decrease in renal blood flow and glomerular filtration rate in patients of renal dysfunction.
- Asthma: Asthamatic patients may develop Aspirin-sensitive asthma which is characterized by pansinusitis, eosinophilia, nasal polyposis, and precipitation of asthma and rhinitis attacks after administration of Aspirin. These patients are more prone to severe bronchospasm and fatal anaphylactoid reactions. Cross reactivity between Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) limits therapy with any NSAID in asthmatic patients with a history of aspirin or other NSAID sensitivity, and careful administration in all patients with preexisting asthma. Aspirin desensitization is also attempted in some cases.
- Dialysis: Salicylates (including Aspirin) and their metabolites can be removed from the body by hemodialysis and also peritoneal dialysis. Dosage adjustment is required in case a patient undergoes dialysis.
- Hepatotoxicity: Aspirin (a salicylate) use may result in acute, reversible hepatotoxicity characterized by elevated levels of alkaline phosphatase, serum transaminases, sometimes bilirubin and also hepatic injury which may occasionally lead to encephalopathy or death. Salicylate therapy including Aspirin should be administered cautiously in patients suffering with rheumatic fever, active systemic lupus erythematosus, juvenile arthritis, or preexisting hepatic impairment. Dosage adjustments is required in case of development of liver function abnormalities and elevated levels of serum salicylate concentration (exceeding 25 mg/dL).
- Glucose-6-Phosphate Dehydrogenase (G-6-PD) Deficiency: Aspirin (Salicylate) may result in the development of or intensify hemolysis in patients having deficiency of enzymes namely, pyruvate kinase or glucose-6-phosphate dehydrogenase (G-6-PD). It is therefore recommended to administer Aspirin in such patients with high caution.
- Reye’s Syndrome (sudden brain damage and liver function problems): The use of salicylate drugs, including Aspirin lead to an increased risk of Reye’s syndrome in children with influenza-like illnesses or varicella infections. It is therefore not advisable to administer salicylates in children who are suffering from or are prone to varicella or influenza infections and also during presumed outbreaks of influenza.
- Gastrointestinal (GI) Toxicity: Aspirin is most often associated with gastrointestinal bleeding and mucosal damage. Therapy with Aspirin may result in iron deficiency anemia and reactivation of latent ulcers, development of peptic ulcers, and ulcer perforation. However, patients who have active peptic ulcers or associated with recent GI bleeding predominantly show increased cases of major upper GI bleeding. Aspirin or other salicylates should be administered cautiously in patients (more particular in elder patients) with a history of GI disease or alcoholism and necessitate close monitoring for toxicity. Co-administration of anti-ulcer agents is generally recommended in patients with active peptic ulceration or GI bleeding treated with Aspirin or other salicylates.
Where can I get more information
Your pharmacist or health care provider can provide more information about Aspirin.
Clinical research and current scenario of the drug
- Studies indicate a decrease in cardiovascular events in case of patients with acute coronary syndrome or who are more prone to cardiovascular diseases when Aspirin is given concomitantly with clopidogrel.
- A large number of clinical trials are being undertaken to investigate the role of Aspirin in the prevention of stroke or heart attack.
- Co-administration of aspirin and platelet P2Y12receptor inhibitors plays a crucial role in the antithrombotic treatment in patients suffering with acute coronary syndrome.
- Clinical studies indicate the use of Aspirin in lowering the risk of in situ breast tumors or hormone receptor-positive tumors and reducing the risk of breast cancer in postmenopausal women.
- Studies involving Salicylates (including Aspirin) in humans and animals nullify them as the sole factor in the generation of permanent threshold shift of auditory sensitivity.
- Clinical studies indicate the use of Aspirin in the primary treatment of venous thromboembolism in patients undergoing surgery and even in non-surgical situations.
- Research indicate that regular administration of Aspirin may contribute to the risk of stroke even in case of healthy people.
- Study shows that regular consumption of Aspirin brings about a reduction in the risk of bowel cancer as well as other hereditary cancers.
- Clinical studies also advocate the role of Aspirin in reducing breast cancer risk by up to 20%.
References from chemical, biological and toxicological databases
- DrugBank: Acetylsalicylic acid (DB00945). http://www.drugbank.ca/drugs/db00945
- Aspirin | C9H8O4 – PubChem. https://pubchem.ncbi.nlm.nih.gov/compound/aspirin
- Aspirin | C9H8O4 | ChemSpider. chemspider.com/Chemical-Structure.2157.html
- Aspirin: MedlinePlus Drug Information. https://www.nlm.nih.gov/medlineplus/druginfo/meds/a682878.html
- Aspirin and recurrent venous thromboembolism. http://www.ncbi.nlm.nih.gov/pubmed/23482543
- Aspirin Use and Risk of Breast Cancer: Systematic Review and Meta-analysis of Observational Studies. http://www.ncbi.nlm.nih.gov/pubmed/26315555
- Pubmed health. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0000168/
- Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews. http://www.ncbi.nlm.nih.gov/pubmed/24074752
- Aspirin for the prevention of cardiovascular events in patients without clinical cardiovascular disease: a meta-analysis of randomized trials. http://www.ncbi.nlm.nih.gov/pubmed/21742097
- Low-dose aspirin in patients with stable cardiovascular disease: a meta-analysis. http://www.ncbi.nlm.nih.gov/pubmed/18187072
- Aspirin: old drug, new uses and challenges. http://www.ncbi.nlm.nih.gov/pubmed/21062358
- The Discovery of Aspirin’s Antithrombotic Effects. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1894700/
