Contents
What is ecchymosis?
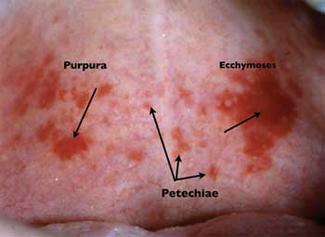
Ecchymosis is described as a large zone of skin discoloration caused by extravasation of blood into the subcutaneous tissue of the body. The term is often mistaken with purpura which is characterized with similar subcutaneous tissue discoloration; however ecchymosis usually refers to a larger, more widespread area.
In addition, ecchymoses, are not necessarily caused by trauma often being provoked by pathophysiologic cell function, and some diseases such as Marburg virus disease. Eccyhmosis is described as a bluish or reddish discoloration of the skin often non-raised and spontaneously caused by a medical condition.
The onset discoloration of the skin is caused by escape of blood from ruptured blood vessels into the capillaries. Ecchymosis is considered as a very important physical sign and finding because it may be related with serious underlying condition. The causes of ecchymosis are various; however, there are certain parts where ecchymosis is important for etiology.
Difference between ecchymosis, purpura, hematoma, petechiae, bruise and hemorrhage
Bruise is a superficial injury produced by impact without laceration.
Hematoma is localized collection of blood that is most usually clotted. It can appear into the organ, tissue or body space due to a blood vessel wall breakage.
Hemorrhage or bleeding is the escape of blood from the vessels.
Petechia is a pinpoint, round, non-raised, purplish to red spot caused by intradermal or submucous bleeding. They are smaller than 1cm in diameter but no larger than 3mm.
Purpura is described as a small reddish purple discoloration of the skin that don’t blanch when external pressure is applied over them. Discolorations are usually small in diameter, measuring anywhere between 3-10 mm and usually have more distinct borders.
Ecchymosis is described as a large zone of skin discoloration caused by extravasation of blood into the subcutaneous tissue of the body.
Ecchymosis discoloration
Discoloration and exact color of the skin represents the physiologic sequel of hemoglobin catabolism which is converted into bilirubin and hemosiderin. Consequently, the tissue gradually changes over time from purple/reddish/black or blue color into to a yellow and green color and at the end into the brownish discoloration. So, ecchymotic region will have different shades of color depending on differential rates of hemoglobin catabolism.
Ecchymosis different types
Ecchymosis caused by some internal conditions can be classified into 4 anatomical areas assigned with an eponym related to the physician who first described the physical finding:
- Skull (Battle sign, Blepharohematoma or Raccoon eye sign)
- Abdominal wall and retroperitoneum (Grey Turner sign Cullen sign Stabler sign)
- Groin and scrotum (Fox, Brian and Stabler sign)
- Lower extremity (Crescent sign)
Such classification is very important for identifying potentially serious risk of internal bleeding. Additionally, these ecchymosis signs may be potentiated by anticoagulation therapy or different platelet abnormalities.
Laboratory and imaging studies done on-time are also very important to further confirm the exact cause of the ecchymosis and guide suitable intervention. It is also important that, that despite careful physical examination, a careful review of the patient’s medications and past medical history be conducted.
Skull ecchymosis
During the examination of an injured patient, it is important to look for and if present, rapidly diagnose a skull base fracture because of its very high morbidity and mortality. In that case computed tomography (CT) imaging is recommended. In some cases condition may prevent prompt and adequate imaging. If skull fracture occurred, in this situation, the physician needs to rely on clinical signs and symptoms.
Two important clinical signs related with fractures of the of the skull base are raccoon eye sign (RES) and Battle sign. Both of these signs are in close connection with a high positive prognostic value for skull fractures and intracranial lesions presence.
Raccoon eye sign trauma or Blepharohematoma
Raccoon Eye Sign Trauma or Blepharohematoma in the frontal region of the skull may be caused by a fracture of the anterior cranial fossa and break of venous structure further leading to bleeding that may extravagate to the regions of the eyelid and orbital adipose tissue. This sign is an important predictive marker for basilar skull fractures as well as for intracranial lesions.
Battle sign ecchymosis
Battle Sign also known as mastoid or retroauricular ecchymosis is a potential clinical marker of the skull base fracture in the posterior cranial fossa. This sign is named after surgeon Dr. William Henry Battle (1855-1936).
According to the data, Battle sign is related with a very positive predictive value of more than 75% cases associated with basilar skull fracture so its presence should raise concern and further diagnosis and the presence of a basilar skull fracture. There are also reports without evident trauma describing a case of hepatic encephalopathy with blepharohematoma and mastoid ecchymosis.
The proposed mechanism of Battle sign manifestation is disruption of the emissary veins that are passing from the sigmoid sinus to the postauricular soft tissue. It has been showed that blunt trauma to the mastoid or temporal bone may result in longitudinal fracture inside the temporal bone.
Other causes that may lead to Battle sign are laceration of the external auditory canal, facial nerve injury, hemotympanum, and transient vertigo. Battle also described that this type of ecchymosis is often first observable 1 to 2 days after the injury and not immediately after the injury. It is likely that the patient with Battle sign will have a slower than expected recovery after head injury.
Abdominal Wall and Retroperitoneum ecchymosis
There have been various signs related with ecchymosis of the abdomen wall or retroperitoneum named after researcher who first described it. But, such signs are potentially markers of a serious internal bleeding so according to the site of discoloration they most commonly named Grey Turner sign which involves the flanks and Cullen sign which involves the umbilicus.
Grey Turner Sign eschymosis
In 1920, George Grey Turner described “dirty-green” discoloration localized on the lateral abdominal wall in one case with acute pancreatitis. The proposed mechanism of this sign manifestation is extraperitoneal blood diffusion from the posterior pararenal space to the lateral edge of the muscle called quadratus lumborum. The presence of this sign in the case of acute pancreatitis is associated with mortality rates of nearly 40%.
Cullen sign ecchymosis
In 1918, Thomas a gynecologist Stephen Cullen (1868–1953) first reported a bluish-discoloration of the periumbilical skin in a woman with a ruptured extrauterine pregnancy. The proposed mechanism of this sign is diffusion of blood from the retroperitoneum to the umbilicus within the falciform abd gastrohepatic ligamen.
So, both Grey Turner and Cullen signs describe that intraperitoneal or retroperitoneal bleeding dissects to the subcutaneous tissue covering the flanks or to the abdominal wall showing skin discoloration.
Moreover, different theories have been suggested in order to explain the chemical properties needed to develop these signs, pointing at a direct role of pancreatic enzymes on the soft tissues and abdominal wall. Approximately, it takes about 3 days for the appearance of Grey Turner’s or Cullen’s sign after the onset of pancreatitis.
Seat belt ecchymosis
The seat belt sign was described as a syndrome by Garrett and Braunstein in 1962 referring to a sustained injury involving the lumbar spine, visceral and solid organ injury, caused by the use of seat belts/lap restraints. In 1968, Doersch and Dozier described this sign as linear ecchymosis of the abdomen or chest wall after motor vehicle accident.
The location of the seat belt signs on the covers the position of the diagonal strap or lap on the seat belt during accident. The contusion is believed to be caused because of mechanistic forces directed to the abdomen or chest during braking or impact.
Groin and scrotum ecchymosis
Groin and scrotum can be also affected. Two most signs are:
- The blue scrotum sign of Bryant
- Stabler Sign
- Fox Sign
The blue scrotum sign of Bryant are described as ecchymosis that is caused by a ruptured abdominal aortic aneurysm extending into the scrotum. However, precise identification of this area caused by ruptured abdominal aortic aneurysm is rare and may involve a region from the anterior abdominal wall, lumbar regions, perineum, scrotum, and in some cases extending to the knee.
The ecchymosis in that case may be continuous or patchy, unilateral or bilateral, and may also involve the lower extremities. This sign is typically manifested 3 or 4 days after the beginning pain symptoms but may be present hours or even weeks after rupture. In some cases, the ecchymosis may look like Grey Turner or Cullen signs.
In the case of Stabler sign, rarely the blood may extravagate and provoke discoloration of the inguinal-pubic area if retroperitoneal hemorrhage occurs. This sign was first described in adult patients with acute pancreatitis with hemorrhage or in the case of ruptured ectopic pregnancy. It has been reported in different abdominal aortic aneurysm rupture.
While rare, this sign is most frequently identified in newborns secondary to adrenal hemorrhage. Perinatal hypoxia, obstetric injury and sepsis are common causes for neonatal adrenal hemorrhage.
In 1966 Fox described 2 cases where bruising was found in the upper outer parts of the thigh, caused by suppurative acute pancreatitis in first one, and a ruptured abdominal aortic aneurysm in the second one. This sign has been also described in other cases such as: strangulated ileum, reaction to subcutaneous injections, urethral instrumentation and pulmonary infarction.
Lower extremity (Crescent sign) ecchymosis
Good and Pozderac described 4 patients with blood in their knees and an acute synovial rupture syndrome. Both confirmed ecchymosis that reached the ankle, forming a crescent above 1 or both malleoli. The crescent sign is defined as a presence of ecchymosis above 1 or more malleoli provoked by synovial rupture because of knee hemarthrosis.
Hemarthrosis can be caused after the trauma to the knee, after anticoagulant therapy or as a bleeding disorder usually accompanied by painful swelling of the joint. The proposed mechanism of this sign is spontaneous synovial rupture provoked by extravasation of blood over the fascial planes to the calf, extending to the ankle.
This typically results in the disappearance and resolution of the knee effusion followed by pain and swelling in the calf. Therefore, in a patient who presents with swelling and pain of the calf, deep vein thrombosis and synovial rupture should be both considered in the differential diagnoses, with presence of a crescent sign.
Ecchymosis general symptoms
Although symptoms of ecchymosis are generally related with the existing condition that influenced the development of ecchymosis there are some general symptoms:
- Discoloration of the skin that is reddish or purplish.
- Patches that are diameter of an inch or more.
- Pain on the affected site although pain may not always be present in some patients.
- Inflammation of skin surrounding the site of ecchymosis. Severity depends on the degree of tissue damage.
- Ecchymosis may spread to surrounding areas depending on the severity and location of ecchymosis.
Ecchymosis most common causes
Various factors can cause bleeding under the skin. Most common causes are:
- Injury or trauma
- Allergic reaction
- Viral infection or illness affecting blood clotting (coagulation)
- Thrombocytopenia
- Autoimmune disorders
- Medical treatment, including radiation and chemotherapy
- Anticoagulants such as warfarin or heparin, aspirin, steroids
- Antiplatelet medicines such as clopidogrel (Plavix)
- Bruise birth
- Aging skin
- Leukemia
- Multiple myeloma
- Idiopathic thrombocytopenic purpura
- Henoch-Schonlein purpura
- Septicemia
- Renal and liver diseases
Leukemia and ecchymosis
As a malignancy of the blood cells leukemia may lead to easy bruising and hemorrhage including signs of ecchymosis. The increase in the levels of white blood cells furthermore influences the development of ecchymosis.
Multiple myeloma and ecchymosis
Multiple myeloma is the cancer of plasma white blood cells that are normally found in the bone marrow. The abnormal and uncontrolled growth of white blood cell in the bone marrow may progress to an abnormality in the blood provoking ecchymosis.
Acute renal failure and ecchymosis
The kidney issues to perform its function regularly and excreting waste from the body may cause progression of waste products in the blood. Ecchymosis may be potentially caused when waste materials accumulate in the blood as a result of abnormalities that resulted from the degeneration of the kidney.
Liver cirrhosis and ecchymosis
Liver issues such as liver cirrhosis may also lead to ecchymosis as result of alteration in the blood composition that may happen as a consequence of liver impairment.
Myelofibrosis and ecchymosis
Myelofibrosis is the fibrosis formation in the bone marrow tissue. The development of fibrosis may result to a disruption in the normal production of blood cells and thus provoke ecchymosis.
Vitamin K Deficiency and ecchymosis
Vitamin K deficiency may also be a cause of ecchymosis, along with hemorrhage and purpura. Decrease in vitamin K-dependent clotting factors II, VII, IX, and X are the most probable reason for that. Therapy includes intramuscular injection of vitamin K 5-10mg per day for several days
Snake Bite and ecchymosis
Snake venom contains hydrolytic enzymes that may cause different reactions in the body manifested with systemic and local effects after snake bite. The place of the snake bite rapidly develops: redness, swelling, and also ecchymosis on the skin. Antivenin and antitetanus are good treatment choices.
Bulimia and ecchymosis
Self-induced vomiting is a common cause of condition called bulimia. Hand is put into the mouth until the gag reflex is provoked and vomiting is induced. Because the hand becomes continuously rubbed against the teeth Russell’s sign may be caused manifested with crusted papules on the back of the hand. Clenching of the fist results to ecchymosis of the fingertips and bleeding underneath the nails.
Grain Itch and ecchymosis
Grain itch can be caused by mites seen on hay, wheat, barley, oat, and other cereals that is why farmers are mostly at risk. A small vesicle is itchy reddish papules that are commonly seen on the trunk. Sooner or later, the lesion turns into an ecchymosis once the hemosiderin settles on the site.
Ecchymosis in children
Ecchymosis typically manifested in kids due to an injury of the skin or mucous membrane. For example ecchymosis of the foot usually happens due to falling down while playing. Fights with peers can also give rise to Ecchymosis of the eye or black eyes in many children. The condition can also be seen in neonates. Ecchymosis in neonates may be caused due to Vitamin C deficiency or low counts of platelets – Thrombocytopenia.
Ecchymosis treatment
Non-serious cases of ecchymosis do not need treatment and are usually resolved on their own. However, regular manifestations on the skin along with pain could be a sign of a more serious condition. In that case doctor should be consulted immediately.
The Ecchymosis management is determined by the underlying health problems. Therefore, after adequate treatment of underlying condition, ecchymosis will be resolved. Some treatment options and recommendations may include:
- Rest promotes healing of damaged skin tissues. Many doctors recommend acceptable in case of ecchymosis to help accelerate the healing process
- Applying ice on the affected sites will cause vasoconstriction of the broken blood vessels and may prevents further spreading of ecchymosis to nearby unaffected areas of the skin
- Painkillers such as acetaminophen and other types of analgesics can be used to relieve the pain associated with Ecchymosis. Don’t use other painkillers because NSAID drugs are not recommended.
- Exercises such as stretching and light massage can help promote healing effects and tissue repair. However, caution is needed during massage as it may cause more damage to blood vessels and tissues.
- Discontinue any drugs that may enhance platelet function including aspirin and other NSAIDs or any other drug that may cause low levels of thrombocytes.
- Maintain fluid volume with a balanced electrolyte solution
- Fresh whole blood transusion or platelet transfusions may be neede and life-saving before a definitive diagnosis is been made
Medications that can be prescribed in the case of ecchymosis
Depending on diagnosed condition following drugs may be prescribed:
- Prednisone alone or in combination with other chemotherapy drugs such as vincristine may be prescribed for immune-mediated low platelet counts or so called immune-mediated thrombocytopenia
- Doxycycline antibiotic may be prescribed for infectious causes or until it has been concluded that an infectious agent is not the cause of the low platelet count (thrombocytopenia)
- Desmopressin acetate can be prescribed for mild platelet function defects, such as Type 1 von Willebrand disease.
Adequate diet recommendations for Ecchymosis
- Vitamin C rich food. Take more vitamin C in order to help promote tissue regeneration. Our body doesn’t naturally produce this vitamin that has excellent anti-oxidant and skin regenerative properties. Adding vitamin C rich foods in your diet will accelerate the healing process for Ecchymosis and other skin conditions. The recommended vitamin C intake is 90 mg/day for men and 75 mg/day for women. Vitamin C rich food may include: unsweetened vitamin C-fortified drinks, tomato juice, spinach, watermelons, green or red pepper, lemon, fresh pineapples, and cantaloupe.
- Foods rich in Vitamin K. Another important vitamin that can help faster healing of Ecchymosis is Vitamin K. Deficiency of this vitamin can decrease the appropriate blood’s clotting ability after experiencing a cut or a bruise. Vitamin K supplementation can help promote normal blood clotting, thus relieving the symptoms of ecchymosis. The recommended daily dose of vitamin K is 90 to 120 micrograms for adults. Foods rich in vitamin K may include: spinach, kale, leafy Swiss chard, broccoli, pasta, olive oil, and canola oil.
- Food rich in Folate. Folate may also promote fast healing of bruises including Ecchymosis thus folic acid is often recommended for patients with Ecchymosis in order to promote quick recovery. Folates are very important role in cell reproduction and tissue regeneration. The recommended daily dosage for folates is 400 g for adults and less than 400 grams for minors. During pregnancy, in case of malasbsorption disorders, and alcoholism folate deficiency may occur. Food rich in folates are: nuts, legumes, fruits, and folic acid fortified foods.
- Vitamin B-12 rich food. A diet containing foods rich in vitamin B12 can help with faster healing of bruises and ecchymosis. Vitamin-B12 rich foods may promote the production of platelets, which are important for clotting. Vitamin B12 deficiency is common in vegetarians, the elderly, during pregnancy and in patients suffering from anemia and different gastrointestinal diseases. The recommended daily intake for vitamin B12 is 2.4 micrograms. Examples of foods rich in vitamin B12 may include: liver, eggs, low fat milk, chicken, fortified cereals, and fish.
“Livedo Reticularis (Mottled Skin) – Definition, Causes, Types, Diagnosis, Cure and Images“