Contents
- What is GHB?
- Is GHB also naturally occurring substance?
- What is Xyrem?
- GHB IUPAC name, chemical structure, mass, formula
- GHB history of use
- GHB legal status
- What are the street names for GHB?
- How GHB looks like?
- Epidemiology of GHB abuse
- GHB physiology in the body
- GHB mechanism of action
- Does GHB affect growth hormone release?
- Why is GHB considered as a date-rape drug?
- GHB illicit manufacturing
- GHB abuse
- GHB addiction and tolerance
- GHB dose-effects
- GHB physical effects
- How can GHB cause both stimulation and sedation?
- GHB cognitive effects
- GHB side effects
- Can GHB overdose cause coma and death?
- GHB withdrawal
- How long GHB stay in the system?
- Why abusers don’t feel ok after even after GHB full elimination?
- Does GHB show up on commercial drug tests?
- GHB detection and testing
- GHB intoxication treatment
- Are there any antidotes for GHB poisoning?
- GHB analogues and their abuse
- Can GHB be taken together with depressant drugs (1,4-Butanediol, 2M2B, alcohol, benzodiazepines, barbiturates, GHB/GBL, methaqualone, opioids)?
- Can GHB be taken together with stimulant drugs?
- Can GHB be taken together with dissociative drugs?
- GHB and alcohol interaction
- GHB and different drugs interactions
What is GHB?
GHB or Gamma Hydroxybutyrate is also known as γ-Hydroxybutyric acid, and 4-hydroxybutanoic acid is a sodium salt drug most commonly known by the trade name Xyrem. It is a prescription sleep-aid which is used to treat numerous medical conditions including cataplexy and excessive daytime sleepiness in patients with narcolepsy. It is also indicated in a medical setting as a general anaesthetic to treat conditions such as insomnia, clinical depression, and alcoholism, and to improve athletic performance.
Is GHB also naturally occurring substance?
Yes, GHB is also a naturally-occurring molecule and metabolite of the strongest inhibitory neurotransmitter gamma-aminobutyric acid (GABA) found in the brain. However, the naturally-occurring metabolite GHB is present in much lower concentrations in the brain than those levels found when the drug is abused. As a result of fermentation, natural GHB may also be found in small but insignificant quantities in some beers and wines.
What is Xyrem?
Xyrem is a brand name prescription drug for sodium oxibate which was approved by the FDA in 2002 for the treatment of narcolepsy, a sleep disorder that causes excessive sleepiness and recurring daytime sleep attacks. It is the sodium salt of gamma hydroxybutyrate.
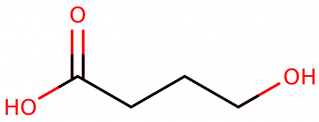
GHB IUPAC name, chemical structure, mass, formula
IUPAC name: 4-hydroxybutanoate
Other (trade) names: γ-Hydroxybutyric acid, G, Sodium Oxybate
Molecular formula: C4H8O3
Molecular weight: 103.09 g/mol
Molecular structure:
GHB history of use
Although Saytzeff isolated GHB in 1874, the first synthesis of GHB occurred during the early 1960s, when Henry Laborit searched for an active, synthetic analogue of GABA that readily crossed the blood-brain barrier and persisted longer than GABA. Early uses of GHB included anesthesia and sleep-induction. In 1962, Blumenfeld et al reported the first use of GHB for surgical anesthesia in humans.
Although GHB was an effective anesthetic with minimal cardiorespiratory depression, recognition of undesirable postoperative sequelae (nausea, vomiting, myoclonus, Cheyne – Stokes respirations), lack of muscle relaxation, and poor analgesia limited the use of GHB as an anaesthetic.
Before 1990, GHB was sold as a dietary supplement in the United States that was a replacement for L- tryptophan. In the United States, reports of enhanced growth hormone release and potential anabolic effects resulted in the misuse of GHB by body builders during the early 1990s; however, the lack of scientific support for the anabolic effects of GHB resulted in the subsequent reduction of GHB use for anabolic purposes.
In the 1990s, the discovery of the euphoric, sedative, and short- term growth hormone- releasing properties of GHB in the club drug and bodybuilding scenes resulted in the popularization of GHB as a substance of abuse. However, case reports associated serious toxic effects (coma, seizures) with the recreational use of GHB.
GHB legal status
The US Food and Drug Administration (FDA) issued a recall for GHB and GBL- containing nutritional supplements in early 1999. The Hillory J. Farias and Samantha Reid Date-Rape Drug Prohibition Act of 2000 reclassified GHB as a schedule I controlled substance as a result of reports of physical dependence and withdrawal following chronic GHB and the use of GHB for sedation and anterograde amnesia during drug-facilitated sexual assaults.
GHB became a controlled substance in most European Union member states in 2001. Amendments to the US Controlled Substances Act allowed the clinical development of sodium oxybate (i.e., oral formulation of GHB) to proceed via a unique, bifurcated schedule. Subsequently, the FDA approved the use of sodium oxybate for the treatment of cataplexy in 2002 as a schedule II drug.
In 2005, the FDA extended the therapeutic use of sodium oxybate (GHB) to include the treatment of excessive daytime sleepiness in patients with narcolepsy. The treatment of cataplexy in adult patients with narcolepsy was approved in the European Union in 2005.
Legal status of GHB in different countries:
- Australia:GHB, 1,4-B and GBL are all Class B illegal drugs, along with any possible esters, ethers and aldehydes.
- Chile:GHB is a controlled drug under the law “Ley de substancias psicotropicas y estupefacientes” (psychotropic substances and narcotics).
- Hong Kong:GHB is regulated under Schedule 1 of Hong Kong’s Chapter 134 Dangerous Drugs Ordinance.
- New Zealand:GHB, 1,4-B and GBL are all Class B illegal drugs, along with any possible esters, ethers and aldehydes.
- Norway:GHB is considered a narcotic and is only available by prescription under the trade name Xyrem.
- Switzerland:GHB is considered a narcotic and is only available by prescription under the trade name Xyrem.
- United States:GHB was placed on Schedule I of the Controlled Substances Act in March 2000. However, when sold as sodium oxybate, it is considered a Schedule III substance but with Schedule I trafficking penalties.It is one of several drugs that are listed in multiple schedules.
- United Kingdom:GHB was made a Class C drug in June 200
What are the street names for GHB?
The street names for GHB are: Liquid X, Liquid ecstasy, Georgia home boy, Oop, Gamma-oh, Grievous bodily harm, Mils, G, Liquid G, Fantasy
How GHB looks like?
GHB appears on the illicit market as a clear, odorless, oily liquid, a crystalline powder, or a gel (sodium salt). The liquid form has a slightly salty taste; occasionally, food dyes or cinnamon are added to improve palatability. The colorless, odorless, highly water soluble properties of the liquid allows the surreptitious use of GHB in the drinks of drug – facilitated sexual assault victims.
Epidemiology of GHB abuse
Illicit GHB use in the United States declined dramatically following the scheduling of GHB as a schedule I controlled substance; GHB exposures reported to the California Poison Control System decreased 76% from 1999. Based on Drug Abuse Warning Network (DAWN) data, approximately 0.3 – 0.4% of drug – related emergency department (ED) visits in the United States are associated with GHB or GHB analogues.
Data from the 2004 National Drug Strategy Household Survey indicated that the prevalence of GHB use was relatively low in Australia. About 0.5% of Australians aged 14 years or older reported the use of GHB at least once in their lifetime and 0.1% reported recent use. The prevalence of GHB use was highest among 20 to 29 year olds. Although
GHB physiology in the body
GHB is a natural constituent of the brain that is both a precursor and metabolic product of GABA. GHB occurs in micromolar quantities (1 – 4 μM ) in all parts of mammalian brains and some peripheral organs (heart, kidney, liver, muscle, brown fat), but the highest GHB concentrations appear in the cytosolic and synaptosomal fractions of the striatum, particularly in the developing brain.
GABA is the major precursor of GHB, and the GHB concentrations in the brain are approximately 0.1% of the GABA concentrations. Synthesis of GHB occurs throughout the central nervous system (CNS), where GHB is released into the synaptic cleft from storage vesicles by potassium – dependent depolarization; then, GHB uptake into the nerve terminal occurs.
GHB synthesis primarily involves the conversion of GABA to succinic semialdehyde via mitochondrial GABA transaminase and the subsequent reduction of succinic semialdehyde to GHB via cytosolic succinic semialdehyde reductase.
GHB mechanism of action
Although GHB is biologically active and ubiquitous in the CNS, the exact mechanism of action is unclear. Experimental evidence suggests that GHB acts as a presynaptic, G- protein coupled neurotransmitter and/or a neuromodulator of the GABA B receptor, particularly in the mesocorticolimbic dopamine pathways.
Most physiologic and pharmacologic effects of exogenous GHB probably result from modulation of GABA B receptors directly as a partial agonist and indirectly through GHB – derived GABA, however, drug discrimination studies suggest that some subtypes of the GABA A and GABA B receptors are also involved as a result of the differences in effect between the GABA B receptor agonist, baclofen, and GHB. GABA B receptors mediate slow inhibitory postsynaptic potentials by activation of calcium channels and G – protein-coupled, inwardly rectifying potassium channels via signaling through the adenylate cyclase system.
GHB binding sites occur throughout the brain including the hippocampus, dentate gyrus, olfactory system, nucleus accumbens, septum, caudate putamen, substantia nigra, ventral tegmental area, pons, and the cortex with lower concentrations of binding sites in the amygdala and the thalamus. Under endogenous conditions, GHB can increase or decrease neuronal activity by inhibiting the release of neurotransmitters located near the endogenous source of GHB.
Does GHB affect growth hormone release?
According to some clinical studies, administration of 2.5 – 3.5 g GHB at bedtime doubles growth hormone secretion, primarily during the first 2 hours after sleep onset. The stimulation of growth hormone secretion correlated to an increase in the amount of sleep stage IV (slow wave, nonrapid eye movement sleep).
However, the exact mechanism of growth hormone release remains unclear as other neurotransmitter pathways (serotonergic, cholinergic) may affect the increased growth hormone release associated with GHB administration.
Additionally, the physiologic importance of growth hormone release remains unclear because there is no direct evidence that short- term elevation in growth hormone increases muscle mass and GHB use does not increase the muscle mass of alcoholic patients.
Why is GHB considered as a date-rape drug?
GHB is available as an odorless, colorless drug that may be combined with alcohol and given to unsuspecting victims prior to sexual assaults. It may have a soapy or salty taste. Use for sexual assault has resulted in GHB being known as a “date rape” drug. Victims become incapacitated due to the sedative effects of GHB, and they are unable to resist sexual assault.
GHB may also induce amnesia in its victim. Common user groups include high school and college students and rave party attendees who use GHB for its intoxicating effects. They are also referred to as “K.-o.-Tropfen” (K.-o.-drops) in German-speaking countries. Care should be taken when offered drinks from strangers.
For GHB use during a drug-facilitated sexual assault, existing studies suggest that GHB use in this setting is uncommon (<3 %), similar to the use of flunitrazepam.
In a systematic review of 11 studies on the involvement In a systematic review of 11 studies on the involvement of GHB in reported sexual assaults, the range of detectable GHB concentrations in reported sexual assaults was 0.2 – 4.4%. However, the short window of GHB detection limits conclusions regarding the prevalence of GHB use during a drug-facilitated sexual assault.
GHB illicit manufacturing
The illicit manufacture of GHB involves the heating of a GBL mixture alkalinized with lye. After the addition of acetone, the mixture is dried. The ester hydrolysis of γ – butyrolactone produces clear solutions containing an amount of GHB equivalent to about 70% of the GBL weight.
Much of the GHB found on the streets or over the Internet is produced in illegal labs. GHB may be adulterated with unknown contaminants that may worsen its toxicity. The production of GHB usually involves the use of lye or drain cleaner mixed with GBL, a chemical cousin of GHB and an industrial solvent often used to strip floors.
GHB abuse
By the late 1990s and early 2000s, GHB was a popular club drug that was associated with the drug-facilitated sexual assault. The use of GHB at party settings appears more common among men than women, and the use of GHB frequently occurs in polydrug users. However, according to some data, private homes are a more common venue for GHB use than nightclubs.
Reports from GHB users describe the effects of GHB as similar to sedative-hypnotic or alcohol intoxication, and chronic use may cause tolerance and dependence. Desirable effects associated with the GHB use recreationally include euphoria, relaxation, loss of inhibitions, increased sociability, better mood, and enhanced sexual awareness.
Although increased sexual desire, arousal, and activity are often related to GHB use, the use of GHB is also associated with decreased sexual performance and impaired memory of the sexual experience. Visual or auditory hallucinations and involuntary limb movements are not typically associated with GHB use.
Preclinical studies of GHB suggest that the abuse potential of GHB is relatively low; however, GHB abuse is a reported complication of the treatment of alcohol dependence/withdrawal with GHB. One study indicated that the abuse likelihood of GHB is lower than pentobarbital and greater than triazolam. Memory impairment was less with GHB compared with pentobarbital or triazolam, and GHB produced significantly greater adverse effects (e.g., nausea).
GHB addiction and tolerance
GHB is moderately physically and psychologically addictive drug. The frequent use of GHB can cause withdrawal symptoms similar to those caused by other depressants such as alcohol and benzodiazepines if abruptly discontinued.
These symptoms seem to depend on the dosage and the length of time the drug was used for. Light to moderate users often experience anxiety, insomnia, sleep-related problems, and tremors whereas heavy use can cause severe withdrawal symptoms like delirium, psychosis, and hallucinations.
Tolerance will develop to the sedative-hypnotic effects within several weeks of continuous use. After cessation, the tolerance returns to baseline in 7 – 14 days.
GHB dose-effects
- For the treatment of narcolepsy, the standard dose of sodium oxybate is 4.5– 9 .0 g at bedtime.
- Single oral doses of 10 mg GHB/kg produce short-term amnesia and hypotonia,
- The ingestion of 20 – 30 mg/kg causes drowsiness.
- In clinical trials, therapeutic doses of GHB for the induction of sleep typically range from 15– 30 mg/kg with doses up to 30 – 50 mg/kg producing sleep that is reversible by external stimulation compared with 50 – 150 mg/kg for the treatment of alcoholics in withdrawal.
- Euphoria may occur at GHB doses used to induce sleep.
- GHB doses above 60 mg/kg are associated with obtundation and coma.
- Intravenous GHB doses of 60 – 70 mg/kg induce sleep within 5 – 15 minutes and coma lasting about 1 – 2 hours followed by rapid arousal. Adverse effects at these doses include nausea, vomiting, hypotonia, bradycardia, respiratory depression, and Cheyne – Stokes respiration.
- The typical street dose of GHB is 2-6 g (25 – 75 mg/ kg or approximately ½ – 1 ¼ teaspoon of pure GHB), but experienced users may ingest up to 30g.
Dose-effects:
- Light effects – 0.5 – 1 g
- Common effects – 1-2 g
- Strong effects – 2-5 g
- Heavy effects – 5-10+ g
GHB physical effects
GHB can provoke following physical effects:
- Stimulation and Sedation
- Respiratory depression
- Dehydration
- Dizziness
- Euphoria
- Motor control loss
- Nausea
How can GHB cause both stimulation and sedation?
At lower doses, GHB is physically stimulating, encouraging movement and wakefulness. At higher doses, however, it becomes physically sedating, encouraging sleep and lethargy.
GHB cognitive effects
GHB can provoke following cognitive effects:
- Disinhibition
- Anxiety suppression
- Empathy, affection, and sociability enhancement
- Memory suppression
- Amnesia
- Euphoria
- Increased libido
- Increased music appreciation
- analysis suppression
- Thought deceleration
- Suggestibility enhancement
GHB side effects
Adverse effects associated with the illicit use of GHB are highly variable; symptoms include euphoria, sedation, memory loss, nausea, vomiting, and lightheadedness. As the dose escalates, agitation, confusion, hallucination, loss of peripheral vision, myoclonus, bradycardia, mild hypothermia, respiratory insufficiency, hypotension, and coma occur, particularly following the concomitant administration of other drugs.
Additionally, GHB use commonly occurs with the use of other drugs of abuse associated with seizure activity. The onset of action following oral GHB administration is rapid (15 – 30 min), while the duration of action of GHB is relatively short.
Based on questionnaires, the acute effects of a single recreational dose of GHB persists about 2– 4 hours (range, < 2 – 6 h). The patient frequently demonstrates anterograde (i.e., after onset of alteration of consciousness), but not retrograde amnesia (i.e., prior to administration).
Can GHB overdose cause coma and death?
Yes, it can. The duration of the coma is relatively short with rapid awakening. Even deeply comatose patients awaken within 4 – 6 hours after ingestion. Recovery typically is spontaneous, frequently abrupt, and often associated with an emergence phenomenon (myoclonic jerks, transient confusion, combativeness).
In a case series of 5 unconscious patients presenting to an ED, the GCS remained unchanged for a median time of 60 minutes (range, 20 – 110 min). Awakening from the coma was rapid (median, 30 min; range, 20 – 60 min).
Death following the ingestion of GHB alone is uncommon, and GHB- associated fatalities usually occur in the setting of polydrug use outside the hospital including abuse of sodium oxybate. Patients with GHB intoxication typically survive if they arrive at the emergency department without anoxic brain damage. Potential causes of GHB – associated deaths include aspiration, respiratory depression, and traumatic injury.
GHB withdrawal
Withdrawal symptoms may occur following the use of prolonged, high – doses of GHB within 1-6 hours following the cessation of GHB use. Typically, these withdrawal symptoms develop in individuals using GHB every 1 – 3 hours; whereas the daily use of GHB during the treatment of narcolepsy is not usually associated with withdrawal.
The minimum daily GHB dose causing withdrawal is difficult to predict because of recall bias and the variable concentrations of GHB in illicit materials. The clinical features of GHB withdrawal are similar to ethanol and sedative-hypnotic (benzodiazepine, barbiturate) withdrawal, but the onset of symptoms (anxiety, delirium) occurs much sooner (< 6 – 12 h) after cessation of use.
The symptoms associated with GHB withdrawal are highly variable, depending primarily on the daily dose and frequency of use. The presentation of the GHB abstinence syndrome includes nausea, vomiting, anxiety, tachycardia, insomnia, tremor, agitation, diaphoresis, and hallucinations; rarely withdrawal symptoms progress to delirium, primarily in severely dependent patients.
In a review of 38 published cases of GHB withdrawal, a majority of patients had tremor, tachycardia, anxiety, hallucinations, and delirium. Seizures do not usually occur during GHB withdrawal. The withdrawal syndrome progresses over the first 2 – 3 days with mild autonomic instability (diaphoresis, hypertension, tachycardia, tremor), anxiety, and hallucinations.
Confusion, disorientation, agitation, or combative behavior may require restraint and sedation. Symptoms of withdrawal typically resolve within 3 – 12 days, but may persist up to 15 days. Case reports suggest that insomnia, anxiety, dysphoria, and poor memory may persist for several months after withdrawal.
How long GHB stay in the system?
To accurately define how long GHB is likely to remain in plasma after discontinuing treatment, it is essential to know its elimination half-life time. GHB is understood to have an elimination half-life time within the range of 20 to 60 minutes after oral use; this is extremely short compared to most medications.
Therefore, it can be estimated that it’ll take up to 1 hour (on average) for your body to eliminate 50% of an ingested GHB dose from plasma circulation. With this data, it can be estimated that it’ll take (on average) between 1.83 and 5.5 hours to eliminate 100% of the GHB from systemic circulation.
Although, GHB is out of your system within just 5.5 hours (on average), does not mean that your neurochemistry will have normalized and/or readjusted back to pre-GHB homeostasis.
Why abusers don’t feel ok after even after GHB full elimination?
It may take a while for neurochemistry to get balanced to homeostatic functioning after GHB usage. During this recalibration phase, the abuser may mistakenly believe that GHB is somehow still in systemic circulation. The true story is that while GHB was in the system, it induced a cascade of potent neurophysiological changes, but was rapidly eliminated.
After its elimination, the abuser may not feel “normal” because his/her neurochemistry hasn’t readjusted itself back to homeostatic functioning. As a result of this altered neurochemical state, abuser will perhaps wrongfully perceive that GHB is still in the system.
Just know that the GHB was likely eliminated within the first half-day (12 hours) post-ingestion and that abuser depersonalization is a lingering byproduct of the changes it made to your neurochemistry while it was in your system.
Does GHB show up on commercial drug tests?
Many individuals are worried that they’ll fail a drug test after taking GHB. However, in the majority of cases, drug tests for GHB will not be administered. Standard drug tests (e.g. SAMHSA-5), and even more extensive screenings do not typically assess for GHB unless specifically requested. Even in the rare case that an individual is subject to GHB testing, he/she is unlikely to test positive due to its rapid elimination half-life.
GHB detection and testing
Rapid colorimetric methods are available to determine the presence of GHB and GBL in urine samples using the ferric hydroxamate test. The limit of detection (LOD) with this method is 0.1 mg/mL in a 1 mL urine sample; this test does not distinguish between GHB and GBL. Positive samples turn purple.
More sophisticated qualitative methods for the detection of GHB and GBL include gas chromatography/flame ionization detection. This method can detect both compounds by the analysis of samples with and without acid hydrolysis to convert GHB to GBL. The LOD is 0.5 mg/L.
Other screening methods that lack sensitivity at low, endogenous GHB concentrations include H nuclear magnetic resonance spectroscopy, micellar electrokinetic chromatography, capillary zone electrophoresis with indirect ultraviolet absorption, and high performance liquid chromatography with ultraviolet or ultraviolet – visible spectrophotometry. Commercial immunoassays for the detection of GHB are generally unavailable.
Many illicit samples of GHB may contain GBL; analysis of illicit samples for GHB precursors by gas chromatography/mass spectrometry or high performance liquid chromatography/ultraviolet – visible spectrophotometry (e.g., GBL, 1,4 – butanediol, maleic anhydride) provides information regarding the origin of the sample.
GHB intoxication treatment
The management of GHB intoxication typically involves stabilization of the airway, support of respirations, and prevention of aspiration. Because of the alteration of consciousness typically associated with GHB intoxication, these patients require monitoring of oxygenation with pulse oximetry and if needed, arterial blood gases.
Supportive care includes supplemental oxygenation, suctioning and positioning for spontaneous vomiting, cardiac monitoring (primarily for bradycardia) and IV access. The mouth should be inspected for the presence of mucosal ulcerations suggestive of alkali burns from the sodium hydroxide used to synthesize GHB.
If present, the patient should be evaluated for the possibility of serious pulmonary complications from aspiration of alkali material. Intubation is usually unnecessary unless hypoventilation, hypoxemia, or the absence of a gag reflex occurs.
When indicated, rapid – sequence intubation usually requires the only paralysis with succinylcholine because of the sedation and amnesia associated with GHB intoxication. The hypothermia associated with GHB use is typically mild and responds well to passive warming techniques.
Measures for gastrointestinal (GI) decontamination (e.g., lavage, activated charcoal) are not routinely recommended for GHB intoxication alone because of the rapid absorption of GHB and potential for aspiration secondary to altered consciousness. The decision to use GI decontamination depends on the clinical severity of other ingested substances.
Are there any antidotes for GHB poisoning?
There are no specific antidotes for GHB intoxication, and naloxone should be administered only for the concomitant presence of opiate intoxication. Experimental studies and case reports indicate that flumazenil does not reverse the clinical effects of GHB.
Although case reports and observational studies suggest that low doses of physostigmine may attenuate the coma associated with severe GHB intoxication, there is insufficient scientific evidence to support the use of physostigmine in the treatment of γ – hydroxybutyrate toxicity. Consequently, the routine use of physostigmine is not recommended, particularly in the setting of the frequent presence of other drugs of abuse.
GHB analogues and their abuse
GHB analogues include 1,4 – butanediol (1,4 – BD), γ butyrolactone (GBL), and γ – valerolactone (GVL). Restrictions on the sale and use of GHB during the 1990s resulted in the use of GHB analogues (e.g., 1,4 BD, GBL) as precursors and surrogates of GHB. GBL was sold OTC and through the Internet either alone or with instructions and components for the home synthesis of GHB. After a FDA warning regarding the health risks of γ-butyrolactone, γ – butyrolactone supplements were voluntarily recalled in 1999. Subsequently, 1,4 – BD products were marketed as replacements for γ – butyrolactone.
GBL and 1,4 – BD is more potent in animal studies than GHB based on the D 50 (dose at which the response decreases by 50%). In a study of rats, the D 50 for GBL, 1,4 – BD, and GHB were 116 mg/kg, 151 mg/kg, and 297 mg/kg, respectively.
A case series of adverse events from 1,4 – BD use associated the ingestion of approximately 1 g 1,4 – butanediol with diaphoresis, confusion, agitation, ataxia, and myoclonus without any clinically significant alteration in vital signs, whereas the ingestion of about 6 – 8 g 1,4 – BD was associated with loss of consciousness, urinary incontinence, vomiting, and mild bradycardia.
In this report, the estimated ingestions of 1,4 – BD by a man and woman found dead in 2 separate incidents were 5.4 g and 20 g based on history from companion.
Can GHB be taken together with depressant drugs (1,4-Butanediol, 2M2B, alcohol, benzodiazepines, barbiturates, GHB/GBL, methaqualone, opioids)?
A review of the details of 194 deaths attributed to or related to GHB over a ten-year period found that most were from respiratory depression caused by interaction with alcohol or other drugs. In humans, GHB has been shown to inhibit the elimination rate of alcohol. This may explain the respiratory arrest that has been reported after ingestion of both drugs.
These substances potentiate the muscle relaxation, sedation and amnesia caused by one another and can lead to unexpected loss of consciousness at high doses. There is also an increased risk of vomiting during unconsciousness and death from the resulting suffocation
The combination of depressants and GHB potentiates amnesia, sedation, and respiratory depression and the muscle relaxation caused by one another. If these drugs are taken in higher doses, it can lead to a sudden, unexpected loss of consciousness along with a dangerous amount of depressed respiration.
There is also an increased risk of vomiting while unconsciousness and dying from the resulting suffocation. If nausea or vomiting occurs before a loss of consciousness, users should attempt to fall asleep in the recovery position or have a friend move them into it.
Can GHB be taken together with stimulant drugs?
It is always dangerous to combine stimulants with depressants drugs such as GHB due to the risk of accidental excessive intoxication, because stimulants mask the sedative effect of depressants, which is the key factor most people use to gauge their level of intoxication.
Once the stimulant effects are off, the depressant effects will significantly increase, leading to motor control loss, intensified disinhibition and dangerous black-out states.
This combination can also potentially result in severe dehydration if fluid intake is not closely monitored. If choosing to combine these substances, one should strictly limit themselves to a pre-set schedule of dosing only a certain amount per hour until a maximum threshold has been reached.
Can GHB be taken together with dissociative drugs?
A combination of GHB and a dissociative drug can unpredictably potentiate the motor control loss, amnesia, sedation, and delusions that can be caused by each other. It may also result in a sudden loss of consciousness accompanied by a dangerous degree of respiratory depression. If nausea or vomiting occurs before consciousness is lost, users should attempt to fall asleep in the recovery position or have a friend move them into it.
GHB and alcohol interaction
The illicit use of GHB frequently occurs with the ingestion of other drugs, particularly ethanol; GHB and ethanol share similar sedative effects. In a double-blind, placebo-controlled, crossover study, 16 healthy adults received GHB (50 mg sodium oxybate/kg) and/or ethanol (0.6 g/kg, estimated blood ethanol concentration 50 mg/dL).
The combination of GHB and ethanol produced more significant adverse effects (vomiting, decreased blood pressure, and reduced oxygen saturation) compared with placebo or each drug alone. However, there were minimal pharmacokinetic interactions (i.e., no statistically significant reduction in elimination half- life or maximal plasma GHB concentrations).
GHB and different drugs interactions
Case reports suggest that concomitant use of human immunodeficiency virus 1 (HIV- 1) protease inhibitors with GHB may exacerbate the respiratory depression and bradycardia associated with GHB intoxication.
Valproate, phenobarbital, barbital, and chlorpromazine inhibit NADPH – dependent aldehyde reductase, which catalyze the formation of GHB from succinic semialdehyde; however, the clinical relevance of this inhibition in regard to GHB concentrations and clinical effects is unclear.