Contents
- What is Levothyroxine
- Generic and brand name of Levothyroxine
- What is the source of the drug (natural or synthetic)?
- Why is Levothyroxine prescribed
- Pharmacophore structure: Information about the chemical structure of the drug
- Chemical information of Levothyroxine
- What are the different dosage forms and strengths of the drug
- How the Levothyroxine medicine works (mode of action)
- How should Levothyroxine be used?
- Recommended doses of Levothyroxine
- What are the pharmacokinetic properties of the Levothyroxine
- What special precautions should I follow/ What should I avoid while using Levothyroxine
- Which pregnancy category (A; B; C; D; X) has been assigned to Levothyroxine
- Levothyroxine Breastfeeding Warnings
- What should I know about storage and disposal of levothyroxine
- What special dietary instructions should I follow
- What should I do if I forget a dose
- What should I do in case of overdose
- Levothyroxine side effects
- Does Levothyroxine have any interaction with other drugs
- Does Levothyroxine have any interaction with Diseases
What is Levothyroxine
Levothyroxine (also known as L-thyroxine) is a synthetic thyroid hormone and chiral compound in the L-form which is chemically identical to thyroxine – T4.
Thyroxine is naturally secreted by the follicular cells of the thyroid gland. Levothyroxine is used for the treatment of thyroid hormone deficiency, and rarely for the prevention of thyroid cancer recurrence.
In the past, its related compound Dextrothyroxine was used for the treatment of hypercholesterolemia but it was withdrawn due to cardiac side effects.
Accordiong to the WHO’s Essential List of Drugs, it is on of the the most important medicine needed in a basic health system. Levothyroxine is also used for the prevention of kidney and eye complications in people who have diabetes.
Generic and brand name of Levothyroxine
- The drug is available under generic name: Levothyroxine Sodium.
- Most common Brand names are: Euthyrox, Synthroid, Levothroid, Levoxyl, Levoxine, Levothyrox, Letrox, Tirosint, and Unithroid.
- This drug can be also used in combination with other drug such as: Np Thyroid 30, Np Thyroid 60, Np Thyroid 90 (containing Levothyroxine and Liothyronine)
What is the source of the drug (natural or synthetic)?
Levothyroxine is a synthetic thyroid hormone. Chemically it is a chiral molecule in the L-form which is identical to natural thyroid prohormone thyroxine – T4.
Why is Levothyroxine prescribed
Levothyroxine is prescribed for:
- Hypothyroidism: Levothyroxine is used as supplemental or replacement therapy in acquired or congenital hypothyroidism of any etiology, except transient hypothyroidism in recovery phase period of subacute thyroiditis. Specific indications include: thyroidal (primary), pituitary (secondary), hypothalamic (tertiary) hypothyroidism and subclinical hypothyroidism. Primary hypothyroidism may result from partial or total congenital absence of the thyroid gland, functional deficiency, primary atrophy, or from the effects of surgery, drugs, radiation, with or without the presence of goiter. Patients with hypothyroidism often require lifelong thyroid hormone therapy
- Pituitary TSH Suppression: In the prevention or treatment of different types of euthyroid goiters including thyroid nodules, subacute or chronic lymphocytic thyroiditis (Hashimoto’s thyroiditis), multinodular goiter and,
- Adjunct therapy for surgery and radioiodine therapy in the treatment of thyrotropin-dependent well-differentiated thyroid cancer.
- It is also used for the treatment of decompensated hypothyroidism or myxedema coma and stupor.
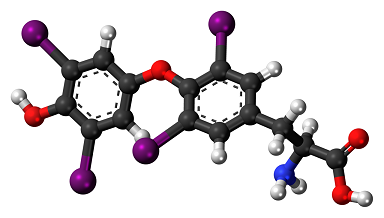
Pharmacophore structure: Information about the chemical structure of the drug
Levothyroxine belongs to the class of organic compounds known as diphenylethers, aromatic molecules containing two benzene rings that are linked to each other with an ether group.
| Kingdom | Organic compounds |
| Super Class | Benzenoids |
| Class | Benzene and substituted derivatives |
| Sub Class | Diphenylethers |
| Direct Parent | Diphenylethers |
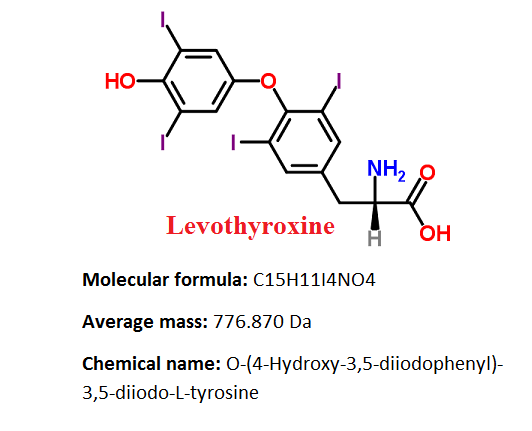
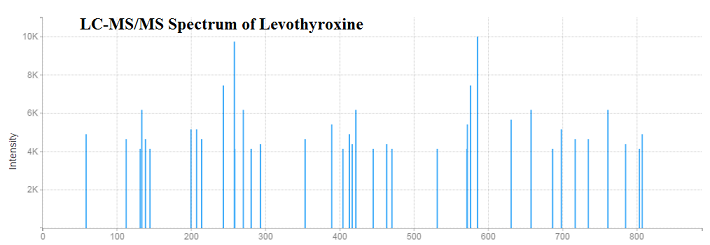
Chemical information of Levothyroxine
- Levothyroxine sodium is an almost white or slightly brownish-yellow powder, or a fine, crystalline powder, which is very slightly soluble in water, slightly soluble in ethanol 96%. It dissolves in dilute solutions of alkali hydroxides.
- Levothyroxine sodium has melting point on 235.5 °C
- Levothyroxine sodium logP value is 4.
What are the different dosage forms and strengths of the drug
Levothyroxine is available in following forms and doses:
- Capsule (13, 25, 50, 75, 88, 100, 112, 125, 137, and 150 ug),
- Liquid (500 mcg), Powder for Solution (200 and 500 mcg) and
- Tablets (100mcg, 100ug, 0.25, 0.5, 0.75, 0,1, 0.2, 0.3, 0.025, 0.05, 0.075, 0.0088, 0.01 mg)
How the Levothyroxine medicine works (mode of action)
Levothyroxine is a synthetically levo-isomer of thyroxine (also known as tetraiodothyronine or T4), which is the main hormone of the thyroid gland. Thyroglobulin releases thyroxine by proteolysis and then hormone is secreted into the blood.
Peripherally, Thyroxine is deiodinated to the form of triiodothyronine (T3) which has a wide spectrum of stimulatory effects on cell metabolism. Thyroid hormones increases the metabolic rate of cells of all tissues in the body.
Thyroid hormone is very significant for the growth and development of all tissues including bones and the brain in the fetus and newborn. In adults, thyroid hormone helps to maintain food metabolism, brain function, and body temperature but also has many indirect effects.
The main symptoms of thyroid deficiency relieved by levothyroxine include lack of energy, slow speech, hair loss, dry thick skin, weight gain, and unusual sensitivity to cold.
Levothyroxine acts by imitating the effects of endogenous thyroid hormone thyroxine – T4, which is a tetra-iodinated tyrosine derivative. T4 is converted to T3 (the active metabolite) in the liver and kidney.
Thyroid hormones attach to thyroid hormone binding proteins, thyroxin-binding globulin, and thyroxin-binding prealbumin (transthyretin) in order to increase solubility.
After that, protein complex is transported to cytoplasm and nucleus of the cell where complex is binding to the thyroid hormone receptors. So by levothyroxine acting as a replacement for natural thyroxine, deficiency symptoms are relieved.
How should Levothyroxine be used?
- Levothyroxine usually comes as a tablet or a capsule to take by mouth. It is usually used once a day on an empty stomach, one half to 1 hour before breakfast. Patients should follow prescribed directions carefully, and ask their doctor or pharmacist any part they do not understand. They should take levothyroxine exactly as directed. They should not take more or less of it or take it more frequently than doctor recommendations.
- Capsules should be swallowed. Capsules should not be chewed or crushed. The tablets may get stuck throat or cause gagging or choking; therefore, the tablet should be taken with a full glass of water.
- If levothyroxine is given to an infant, child, or adult who cannot swallow the tablet, the tablet should be crushed and mixed in 1 to 2 teaspoons of plain water.
- This drug should be taken at least 4 hours before or after administration of other drugs that are known that interfere with its absorption.
- The peak therapeutic effect is expected after 4 to 6 weeks.
- The individualization of the dose should be performed on the basis of clinical response and biochemical test results. Regular monitoring of TSH and thyroxine is recommended at the beginning of therapy or changing the dose.
- Doctor will probably start with therapy on a lower dose of levothyroxine and gradually increase the dose.
- Levothyroxine can control hypothyroidism, make symptoms less frequent but it does not cure it. It may take several weeks before patients can notice a change in their symptoms. Patients should continue taking levothyroxine even if they feel well. Patient should not stop taking levothyroxine without talking to your doctor.
Recommended doses of Levothyroxine
Usual Adult Dose for Hypothyroidism:
Therapy may be started at full replacement doses in otherwise healthy individuals who are less than 50 years old and in those older than 50 years who have been recently treated for hyperthyroidism or who have been hypothyroid for only a short time (few months):
- Average full replacement dose: 1.7 mcg/kg/day (100 to 125 mcg/day for a 70 kg adult)
- Older patients may require less than 1 mcg/kg/day
- Doses greater than 200 mcg/day orally are rarely required
- An insufficient response to daily doses of 300 mcg/day or higher is very rare and may be because of poor compliance, drug interactions or malabsorption.
Patients older than 50 years or patients under 50 years with undrlaying cardiac disease:
- Initial dose: 25 to 50 mcg/day, with gradual increments in dose at 6 to 8 week intervals, if it is needed
Patients with severe hypothyroidism:
- Initial dose:5 to 50 mcg once a day orally; dosage can be increased in 12.5 to 25 mcg/day increments every 2 to 4 weeks (until the TSH level is normalized, accompanied by clinical and laboratory results)
Patients with pituitary – secondary or hypothalamic – tertiary hypothyroidism:
- The oral dose should be titrated until the serum level of free-T4 is restored to normal range and if patient is clinically euthyroid.
-This drug should be taken in the morning on an empty stomach with water, at least one-half hour before any food is eaten.
Usual Adult Dose for TSH Suppression
Patients with thyroid cancer and thyroid nodules:
- The target level for TSH suppression has not been established. For benign nodular disease the efficacy of TSH suppression is controversial. Thus, the dose should be individualized based on the specific disease and the patient being treated.
- In the management of well differentiated thyroid cancer (papillary and follicular), levothyroxine is used as an adjunct therapy to surgery and radioiodine therapy. Generally, TSH is suppressed to less than 0.1 IU/liter (mU/L), and this usually requires a dose greater than 2 mcg/kg/day. However, in patients with high-risk tumors, the target level for TSH suppression may be less than 0.01 mU/L.
- In the treatment of benign nodules and nontoxic multinodular goiter, TSH is generally suppressed to a higher target such as 0.1 to 0.5 mU/L for nodules and 0.5 to 1.0 mU/L for multinodular goiter compared to the doses used for the treatment of thyroid cancer. This drug is contraindicated if the serum TSH is already suppressed due to the risk of precipitating overt thyrotoxicosis.
Usual Adult Dose for Myxedema Coma
Myxedema coma is a life-threatening condition characterized by hypometabolism and poor circulation. It may result in unpredictable absorption from the gastrointestinal tract after oral administration. Only the intravascular dosage form of levothyroxine should be used for this condition:
- Initial dose: 300 to 500 mcg intravacular
- Maintenance dose: 50 and 100 mcg intravascular, until the patient can tolerate oral therapy
Elderly patients with cardiac disease:
- Initial dose:5 to 25 mcg per day orally, with gradual dose increments at 4 to 6 week intervals
- The dose is adjusted in 12.5 to 25 mcg increments until the patient with primary hypothyroidism is clinically euthyroid and the serum TSH has normalized.
Congenital or acquired hypothyroidism:
- Neonatal: 10 to 15 mcg/kg/day.
- Age 0 to 3 months: 10 to 15 mcg/kg once per day orally
- Age 3 to 6 months: 8 to 10 mcg/kg/day
- Age 6 to 12 months: 6 to 8 mcg/kg/day
- Age 1 to 5 years: 5 to 6 mcg/kg/day
- Age 6 to 12 years: 4 to 5 mcg/kg/day
- Age 12 years and older: 2 to 3 mcg/kg/day
- Patients in which growth and puberty are complete: 1.7 mcg/kg/day
- For chronic or severe hypothyroidism: 25 mcg once per day orally and increase dosage as needed in increments of 25 mcg every 2 to 4 weeks until the desired effect is achieved.
What are the pharmacokinetic properties of the Levothyroxine
Absorption: Absorption of levothyroxine after oral administration from the gastrointestinal tract varies from 40–80%, but the most of the drug is absorbed from the jejunum and upper ileum.
Levothyroxine absorption can be increased by fasting and reduced in certain malabsorption conditions, by certain foods, and with age. Dietary fibers can dcrease the bioavailability of the drug.
Distribution: More than 99% of circulating thyroid hormones are bound to plasma proteins such as thyroxine-binding prealbumin, albumin and thyroxine-binding globulin. Only free form of hormone is metabolically active.
Metabolism: About 70% of secreted T4 is deiodinated to equivalent amounts of T3 and reverse triiodothyronine (rT3), which is metabolically inactive. Elimination of T3 and T4 involves metabolic reactions of hepatic conjugation to glucuronic and sulfuric acids.
The hormones go through enterohepatic circulation and after that, they are as conjugates hydrolyzed in the intestine and reabsorbed. Conjugated molecules that reach the colon are hydrolyzed and eliminated as free compounds in the feces. Other minor T4 metabolites have been also identified.
Excretion: Levothyroxine half-life is 6–7 days for healthy patients, 9–10 days for patients with hypothyroidism and 3–4 days for patients with hypothyroidism.
Approximately 80% of thyroid hormones are eliminated by the kidneys; however urinary excretion is decreased with age. The remaining 20% of T4 is eliminated in the feces.
What special precautions should I follow/ What should I avoid while using Levothyroxine
Before taking Levothyroxine:
- Patients should tell their doctor and pharmacist if they are allergic to levothyroxine, or any other medications, or any of the ingredients in levothyroxine dosage forms.
- Patients should tell their doctor and pharmacist what prescription and nonprescription medicines, nutritional supplements, vitamins and herbal preparations they are taking or plan to take. Patients should mention if they are using any of the following drugs: anticoagulants such as warfarin (Coumadin), amiodarone (Cordarone, Pacerone); amphetamines; aspirin or any other NSAID; beta-blockers such as propranolol (Inderal), timolol (Timoptic), metoprolol (Lopressor), carbamazepine (Equetro, Tegretol); corticosteroids such as dexamethasone; imatinib (Gleevac); insulin or other medications to treat diabetes; lithium (Lithobid); maprotiline; oral contraceptives; selective serotonin reuptake inhibitors (SSRIs) such as sertraline (Zoloft); theophylline (TheoDur); and tricyclic antidepressants such as amitriptyline (Elavil), phenobarbital; phenytoin (Dilantin, Phenytek); rifampin (Rifater, Rifamate, Rifadin). Doctor may need to change the doses of these medications or monitor carefully for side effects.
- Patients should also mention their doctor or pharmacist if they are taking: any antacid drug, colesevelam (Welchol), colestipol (Colestid), calcium carbonate (Tums), iron, orlistat (Alli, Xenical), simethicone (Phazyme, Gas X), sevelamer (Renvela, Renagel), sucralfate (Carafate), sodium polystyrene sulfonate (Kayexalate. These drugs have to be taken at least 4 hours after or 4 hours before levothyroxine administration.
- Patients should tell their doctor and pharmacist if they have or have ever had diseases such as: diabetes; atherosclerosis, some liver or kidney disease; bleeding problems; porphyria, cardiovascular disease such as chest pain (angina), arrhythmias, high blood pressure or heart attack; an underactive adrenal or pituitary gland, or any condition that makes swallow difficult.
- Patients should also tell their doctor if they are pregnant or plan to become pregnant or are breast-feeding. If they become pregnant while using levothyroxine, they should call their doctor.
- If patients should have surgery, including dental surgery, they should tell their doctor or dentist that they are using levothyroxine.
Which pregnancy category (A; B; C; D; X) has been assigned to Levothyroxine
Levothyroxine has been given pregnancy category A by the FDA. This means that this drug has no risk during pregnancy – “Adequate and well-controlled human studies have failed to demonstrate a risk to the fetus in the first trimester of pregnancy (and there is no evidence of risk in later trimesters).”
Studies in women using levothyroxine during pregnancy have failed to show an increased risk of congenital abnormalities. Thus, the possibility of fetal harm is excluded. Levothyroxine should not be discontinued during pregnancy and hypothyroidism diagnosed during pregnancy should be treated promptly.
Levothyroxine Breastfeeding Warnings
Although thyroid hormones can be excreted only in small amounts into human milk, caution is needed when Levothyroxine is administered to a nursing woman. However, adequate replacement doses of Levothyroxine are generally required to maintain normal lactation.
What should I know about storage and disposal of levothyroxine
This medication should be kept in the container it came in, out of reach of children and tightly closed. It should be stored at room temperature and away from extra heat and moisture (not in the bathroom). Outdated medications should be thrown away any medication. Patients should talk with their pharmacist about the proper disposal of this medication.
What special dietary instructions should I follow
Patients should eat a normal and healthy diet. Some foods and beverages, particularly those that contain walnuts, dietary fiber and soybeans, may affect how levothyroxine action, so it recommendable to take levothyroxine one half to 1 hour before breakfast.
What should I do if I forget a dose
The missed dose should be taken as soon as patients remember it. However, if it is almost time for the next dose, patients should skip the missed dose and continue the regular dosing schedule. They should never take a double dose to make up for a missed one.
What should I do in case of overdose
In case of overdose, patients should call their local poison control center at 1-800-222-1222. If the victim has collapsed or is not breathing, call local emergency services at 911.
Levothyroxine side effects
The table below shows the incidence of side effects after levothyroxine administration in recommendable doses. The incidence can be increased if this drug is overdosed.
| Frequency not defined | Angina pectoris, Myocardial infarction, Palpitations, Congestive heart failure, Flushing, Increased pulse, Choking sensation, Emotional lability, Headache, Heat intolerance, Arrhythmias, Arthralgia, Alopecia, Weight loss, Infertility, Dyspnea, Tremor, Fever, Tachycardia, Nervousness, Anxiety, Myasthenia, Pseudomotor cerebri, Cramps, Diarrhea, Insomnia, Decreased bone mineral density |
Does Levothyroxine have any interaction with other drugs
Glucocorticoids, Dopamine/Dopamine Agonists and Octreotide: These drugs may reduce TSH secretion however the reduction is not sustained, therefore, hypothyroidism does not occur.
Amiodarone, Lithium, Iodide, Propylthiouracil (PTU), Methimazole, Tolbutamide and Sulfonamides: These drugs may decrease thyroid hormone secretion, which may result in hypothyroidism. However, Iodide and Amiodarone may cause hyperthyroidism in euthyroid patients with Grave’s disease previously treated with antithyroid drugs or in euthyroid patients with thyroid autonomy. Amiodarone may induce hyperthyroidism by causing thyroiditis.
Antacids, Bile Acid Sequestrants, Calcium Carbonate, Cation Exchange Resins, Orlistat
Sucralfate, Ferrous Sulfate: These drugs may reduce T4 absorption, which may result in hypothyroidism.
Furosemide, Hydantoins, Non-Steroidal Anti-Inflammatory Drugs, Salicylates, Heparin: These drugs may cause protein-binding site displacement so co-administration of these agents with Levothyroxine may result in an initial increase in FT4. Continued administration results in a decrease in serum T4 and normal FT4 and TSH concentrations and, therefore, patients are clinically euthyroid.
Clofibrate, Estrogens (oral), Estrogen-containing oral contraceptives, 5-Fluorouracil, Heroin/Methadone, Mitotane, Tamoxifen: These drugs may increase serum TBG concentration.
Androgens/Anabolic Steroids, Asparaginase, Glucocorticoids, and Nicotinic Acid: These drugs may decrease serum TBG concentration.
Carbamazepine, Phenobarbital, Rifampin and Hydantoins: These drugs may increase hepatic metabolism, which may result in hypothyroidism. Stimulation of hepatic microsomal metabolizing enzyme activity may cause increased hepatic degradation of Levothyroxine, resulting in lower concentration of Levothyroxine in blood and thus less effects of the drug
Amiodarone, Beta-adrenergic antagonists and Glucocorticoids: Administration of these drugs may decrease the peripheral conversion of T4 to T3, leading to decreased T3 levels.
Anticoagulants (oral): Anticoagulants and Levothyroxine co-administration may lead to increased catabolism of vitamin K-dependent clotting factors, thus increasing the anticoagulant activity of oral anticoagulants.
Antidepressants: Concomitant use of tri/tetracyclic antidepressants and Levothyroxine may increase the therapeutic and toxic effects of both drugs.
Antidiabetic Agents: Addition of Levothyroxine to antidiabetic or insulin therapy may result in increased antidiabetic agent or insulin requirements.
Cardiac Glycosides: Therapeutic effect of digitalis glycosides may be reduced.
Cytokines (Interferon-α, Interleukin-2): Therapy with interferon-α has been associated with the development of antithyroid microsomal antibodies in 20% of patients and some have transient hypothyroidism, hyperthyroidism, or both.
Growth Hormones: Excessive use of thyroid hormones with growth hormones may accelerate epiphyseal closure.
Ketamine: Concurrent use with Levothyroxine may produce hypertension and tachycardia.
Methylxanthine Bronchodilators such as Theophilline: Decreased theophylline clearance may occur in hypothyroid patients
Sympathomimetics: Concurrent use may increase the effects of sympathomimetics or thyroid hormone.
Radiographic Agents: Thyroid hormones may reduce the uptake of 123 I, 131I, and 99mTc.
Does Levothyroxine have any interaction with Diseases
Bone Mineral Density: In women, prolonged therapy with Levothyroxine has been linked with increased resorption of bone, by decreasing the mineral density of bones, especially in postmenopausal women on greater than replacement doses or in women who are receiving suppressive doses of Levothyroxine.
The increased resorption of the bones may be related with increased blood levels and urinary excretion of phosphorous and calcium, elevations in bone alkaline phosphatase and suppressed PTH-parathyroid hormone levels.
Patients with Cardiovascular Disease: Caution is needed when Levothyroxine is administered to patients with cardiovascular disorders and to the elderly where is an increased risk of cardiac diseases.
In such patients, Levothyroxine should be initiated at lower doses than doses which are recommended in younger and healthy individuals or in patients without cardiac disease.
If cardiac symptoms develop or worsen, the Levothyroxine dose should be reduced or discontinued for one week and then cautiously restarted at a lower dose.
Levothyroxine overdosage may have side cardiovascular effects such on: heart rate, thickness of cardiac wall, and cardiac contractility and may precipitate arrhythmias or angina.
Patients with coronary artery disease who are using Levothyroxine should be monitored carefully during surgical procedures, since the possibility of precipitating cardiac arrhythmias may be greater in those treated with Levothyroxine.
Combination of Levothyroxine and sympathomimetic agents to patients with coronary artery disease may precipitate coronary insufficiency.
Patients with Nontoxic Diffuse Goiter or Nodular Thyroid Disease: When administering Levothyroxine to patients with nontoxic diffuse goiter or nodular thyroid disease caution is needed in order to prevent thyrotoxicosis precipitation. If the serum TSH is already suppressed, Levothyroxine should not be administered.
Hypothalamic or Pituitary Hormone Deficiencies: In patients with secondary or tertiary hypothyroidism, additional hypothalamic/pituitary hormone deficiencies should be considered, and, if diagnosed, treated.
Autoimmune Polyglandular Syndrome: Patients with adrenal insufficiency should be treated with glucocorticoids before the beginning of Levothyroxine therapy.
Failure may precipitate an acute adrenal crisis when therapy with levothyroxine is started, due to increased metabolic clearance of glucocorticoids by thyroid hormone. Patients with diabetes mellitus may require upward adjustments of their antidiabetic therapeutic regimens when treated with Levothyroxine.
Information retrieved from:
http://www.chemspider.com/Chemical-Structure.5614.html?rid=447fc4fa-fddf-4980-9a4f-2da5d2be08b3
http://www.drugs.com/pro/levothyroxine.html
http://www.druglib.com/druginfo/levoxyl/indications_dosage/
https://www.nlm.nih.gov/medlineplus/druginfo/meds/a682461.html
http://www.rxlist.com/levoxyl-drug/indications-dosage.htm
http://www.drugbank.ca/drugs/DB00451
http://reference.medscape.com/drug/synthroid-levoxyl-levothyroxine-342732
http://www.healthnewslibrary.com/most-of-the-population-have-thyroid-problems/