Contents
- What is Tinea versicolor?
- Is Tinea versicolor contagious?
- Tinea versicolor signs and symptoms
- What causes Tinea versicolor?
- How does Tinea versicolor spread?
- Tinea versicolor complications
- Is Tinea versicolor autoimmune disease?
- Is Tinea versicolor hereditary disease?
- Tinea versicolor diagnostic and tests
- Tinea versicolor treatment
- Home remedies for Tinea versicolor
- Tinea versicolor prevention
- Selsun Blue for Tinea versicolor
- What is adequate diet for Tinea versicolor patients?
What is Tinea versicolor?
A type of yeast found on the skin surface is the fungus Malassezia. Usually, no health problems are caused by this organism. In fact, a number of microbial organisms or microbiotas, including yeast species such as Malassezia, survive on the human skin in large colonies.
These provide protection from a number of harmful pathogenic organisms as well as infections. They live successfully along with the cells of the human body, in symbiotic relationships. The microscopic organisms as well as the skin cells benefit as well as support each other.
There are times when the organism might exhibit uncontrolled growth. This can affect the pigmentation of the skin or the natural skin color. Due to this, development of patches on the skin might take place, which are lighter or darker in color, compared to the natural surrounding skin.
This is a non – contagious skin condition, termed as Tinea versicolor or Pityriasis versicolor. The condition occurs due to the infection or suppressed immune response caused by a type of yeast belonging to the family Malassezia.
Is Tinea versicolor contagious?
Patients must acknowledge the fact that the causative agent for Tinea versicolor is a fungus which is normally present on the surface of our skin. Therefore, it cannot be termed as a contagious disease. The sequel caused by the infection do not have a permanent existence.
Additionally, any alterations in the pigmentation resolve completely, after one or two months after the initiation of the treatment. Treatment is required as a remedy for the condition as well as for prophylaxis to prevent the recurrence of the infection.
Tinea versicolor signs and symptoms
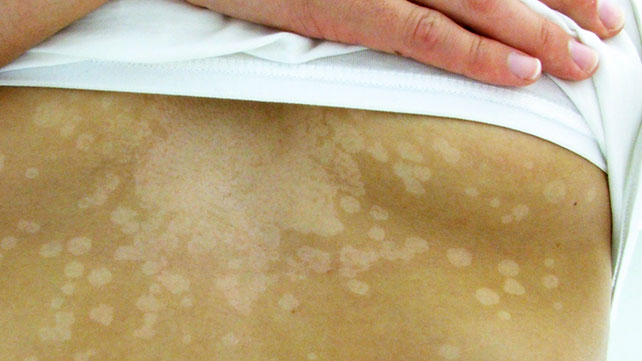
One of the most noticeable symptoms of Tinea versicolor is the presence of discolored patches on the skin. These are usually present on the chest, back, neck and the arms. The patches can be –
- Lighter than normal skin tone (more common) or danker, compared to the surrounding skin
- Tan, red, pink or brown in colour
- Itchy, dry and scaly
- Appear more prominent with tanning
- Are prone to disappear, when the weather is less humid and cooler
Development of Tinea versicolor in people with darker skin complexion can result in the loss of skin pigmentation, a condition often termed as hypopigmentation. In case of some people, darkening of skin might occur, instead of lightening, termed as hyperpigmentation condition.
There are certain individuals who develop Tinea versicolor but do not experience any significant changes in the colour or appearance of the skin. Apart from the change in the skin color, one might experience itchiness in the skin as well.
There are also some other similar conditions which have overlapping symptoms and are often confused with Tinea versicolor. For example, vitiligo is usually mistaken for Tinea versicolor. Yet, there are several differentiating factors between the two –
- The affected individual’s skin texture is not affected by vitiligo
- Appearance of vitiligo is usually on the armpits, fingers, eyes, mouth, wrists or groin
- Usually, symmetrical patches are formed by vitiligo
Pityriasis rosea also causes a rash, which is similar to Tinea versicolor. The difference lies in the fact that the rash is often preceded by a lone red patch of scaly skin, termed as the ‘herald patch’. This appears a few days or weeks prior to the appearance of rash.
The typical shape of the rash on the back is that of a Christmas tree. The reasons or the causative agents of this condition are unknown. But, just like the Tinea versicolor condition, it ceases to be both contagious and harmful.
What causes Tinea versicolor?
Tinea versicolor occurs due to the rapid and uncontrolled growth of Malassezia on the skin surface. Certain factors, as stated below, might favour and promote the growth of the yeast on the skin:
- Excessive sweating
- Hot and humid weather
- A weak immune response/ immune system
- Oily skin
- Changes in the hormonal balance
Individuals from all ethnic backgrounds can suffer from Tinea versicolor and it is more commonly observed in young adults or adolescents. Visiting an area with a subtropical climate makes adults more prone to develop Tinea versicolor.
How does Tinea versicolor spread?
There are a number of environmental as well as biological factors which put an individual on a higher risk of developing the condition:
- Excessive sweating
- Weak immune system
- Family history of Tinea versicolor
- Certain types of cancers
- Consumption of medications which subdue the immune system
Tinea versicolor complications
The Tinea versicolor infection can also cause complications such as:
- Recurrence of the infection
- Even after the treatment of the infection, the patches and scars may remain on the skin for an extended time period
- Individuals who have a weak immune system or are on immunosuppressant drugs have high risk of developing other complications
- Medications used for the treatment of Tinea versicolor may have a side effect on some individuals but this varies person to person
Is Tinea versicolor autoimmune disease?
Unlike psoriasis, which is an autoimmune disease, Tinea versicolor is a fungal infection. It is caused due to the rapid over growth of yeast species. Also, every individual has a certain amount of year living on the skin, so this is just a slight abnormal condition.
Is Tinea versicolor hereditary disease?
Tinea versicolor is a common infection which can infect healthy individuals. The causative agent is afungal specie living normally on human skin. Though its nature is poorly understood, there seems to be a genetic predisposition to the development of the Tinea versicolor infection in individuals.
Tinea versicolor diagnostic and tests
If you experience the development of symptoms of Tinea versicolor or have suspicion regarding the same, you may choose to treat the condition by yourself. OTC (over the counter) antifungal medicines can be used to eliminate any discoloured patches visible on the skin. However, the doctor must be contacted if the treatments seem to be ineffective. Prescription medicines might be required to control the symptoms of the infection in some individuals.
If treating at home is not possible, you must consult the doctor regarding the strangely coloured patches on the skin. The doctors examine the skin and are accurately able to identify if you are suffering from Tinea versicolor, simply by visual examination of the patches.
If visual diagnosis is not possible, a skin scraping can be taken by the doctor. For a skin scraping, removal of some cells from the skin is done, for testing purposes. The skin is gently scraped for the same. By viewing under a microscope, the yeast causing the infection can be identified.
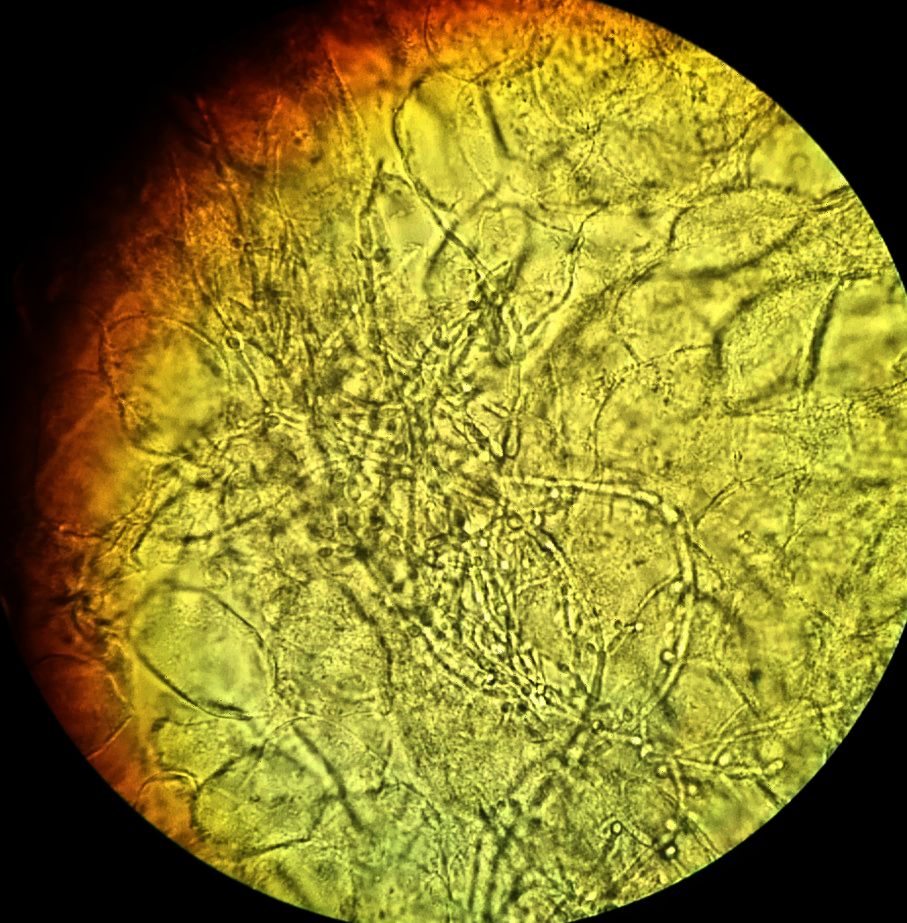
KOH Test in picture below
Alternatively, the doctor might conduct a potassium hydroxide (KOH) microscopy. For this procedure, a skin sample is taken by the doctor, which is further placed on a microscope slide with a 20% potassium hydroxide solution. Further, the doctor or lab technician looks under the microscope for the hyphae fungi or the yeast.
A biopsy can be taken by the doctor (a tissue sample), of the affected skin to test for fungi on the outer surface. Fungal sample can also be alternatively tested in a fungal culture.
A Wood’s lamp can be used by the doctor to visualize the skin. It is a special instrument, which makes use of ultraviolet (UV) light and is held about four to five inches from the skin. In presence of yeast, the skin appears green or yellow under the light.
Tinea versicolor treatment
If there aren’t’ any severe symptoms, you can always choose to treat the infection at home. Over the counter anti fungal shampoos and creams might be effective for killing the infecting organism. The active ingredients in these medications often include ketoconazole, selenium sulphide and pyrithione zinc. Some OTC medications for Tinea versicolor include –
- Selenium Sulfide: Selsun Blue Shampoo
- Miconazole: M-Zole, Monistat
- Clotrimazole: Mycelex, Lotrimin AF
- Terbinafine: Lamisil
In case you wish to seek medical attention for the infection, if the condition is too severe or in cases where the OTC medications are ineffective, different medications might be prescribed by the doctor for Tinea versicolor. These are generally topical creams which need to be directly applied to the affected skin. These are prescription strength medications. A few examples are –
- Ketoconazole: Nizoral, Extina
- Ciclopirox: Penlac, Loprox
Pills may also be prescribed by the physician. Some examples include –
- Itrazonazole: Sporanox, Onmel
- Fluconazole: Diflucan
- Ketoconazole
Even post successful treatment, for weeks or even months, the skin colour might remain uneven. The infection can always make a comeback in hot, humid weather. In some persistent cases, to prevent the infection from recurring, you might be advised to take medication once or twice a month.
Home remedies for Tinea versicolor
- You can apply OTC dandruff shampoos to the affected skin daily in the shower, for about 10 minutes. This is a useful home remedy and you can always consult your doctor regarding the same.
- Some other suggested home remedies include tea tree oil, honey, aloe vera, beeswax, apple cider vinegar and olive oil. Before you try any of these, prefer consulting a dermatologist.
- In a 2004 published study, it was indicated that application of olive oil, honey and beeswax proved beneficial for a number of patients. A mixture of the three, in equal parts was applied by then for a month, about three times per day.
Tinea versicolor prevention
Usually, preventing recurrence of the infection is difficult. After diagnosis and successful treatment of Tinea versicolor, you can take a few steps to prevent infection in future.
- Avoid subtropical or hot and humid climate
- Steer clear of excessive heat
- Avoid excessive sun exposure or tanning
- Try to avoid excessive sweating
You may also opt for a prescription strength skin treatment during the months of the year when susceptibility of recurrence of the infection is high for you.
Selsun Blue for Tinea versicolor
Selsun Blue (selenium sulphide) is a medicated, non prescription shampoo, which is helpful in the Tinea versicolor condition. All you need to do is apply the shampoo once a day for a period of two weeks. You need to apply it to the affected region on the skin as well as 2 to 3 inches area around the spots. Following application by rubbing, allow it to dry.
Make sure that it is kept away from the genitals and the eyes as it might irritate the sensitive tissues. Take a shower after lapse of 10 minutes. The scaling should stop after a period of two weeks and the rashes would be cured, temporarily. For about six to twelve months, the normal skin colour will not return.
- Helps prevent recurrence – Tinea versicolor has a high tendency to recur. You can apply the Selsun Blue shampoo on the previously affected areas once a month for a number of years. Simply apply as per the procedure described above before a shower. It is highly helpful in the summer months, when the fungus thrives.
What is adequate diet for Tinea versicolor patients?
What you must eat and must avoid is necessary to monitor. It is always advisable to follow a proper diet to prevent recurrence.
What to avoid eating?
- Sugar – Both in the simple and complex forms (in various food products), sugar serves as fuel for the growth of yeast and fungal molds. To fight effectively with the microorganism, avoiding sugar is a must.
- Vinegar – Present in ketchup, mayonnaise, salad dressing, etc. It is made from old wine, which is yeast concentrated.
- Barley Malt – Serves as food for yeast growth and is present in various types of bread, as well as grains and cereals.
- Baked food items – Use baker’s yeast
- Fruits and nuts – These are a natural source of natural sugars like fructose
- Alcohol
What to include in the diet to prevent Tinea versicolor recurrence?
- Yogurt
- Raw vegetables and fruits
- Whole grains
- Probiotics
- Garlic