Contents
- What is ketamine?
- What are the street names for Ketamine?
- Ketamine IUPAC name, chemical structure, mass, formula
- Ketamine drug class
- Ketamine chemistry and racemic composition
- Ketamine history of use
- Ketamine legal status
- How does ketamine look like? How is ketamine abused?
- Ketamine mechanism of action
- Ketamine medical uses
- Ketamine dose-effect
- Ketamine effects
- Ketamine side effects
- Ketamine overdose
- Ketamine abuse
- Who abuses ketamine the most?
- Ketamine addiction
- Ketamine abstinence syndrome
- Ketamine withdrawal
- Ketamine absorption, metabolism and excretion
- How long ketamine stay in your system?
- Ketamine drug interactions
- Ketamine intoxication treatment
- Are there some antidotes for ketamine intoxication?
- Can commercial drug tests detect ketamine?
- Ketamine detection in urine, blood, saliva and hair
What is ketamine?
Ketamine is a weakly basic compound structurally and pharmacologically similar to phencyclidine, which is first utilized in the U.S. to induce anesthesia. It is available in solution for intravenous or intramuscular injection. Since the drug is pharmacologically similar to PCP it has the potential of producing hallucinogenic effects and, therefore, in recent years has become a drug of abuse.
It has also been efficacy used for pain control in burn therapy, battlefield injuries, and in children who cannot use other anesthetics due to side effects or allergies. Pharmacologically, ketamine works as a noncompetitive NMDA receptor antagonist, but at higher doses may also bind to the opioid mu and sigma receptors.
What are the street names for Ketamine?
The street names for Ketamine are: Bump, Cat Valium, Green, Honey Oil, Jet, K, Kay, Kay-Blast, Kay Jay, Keets, Keller, Kellys Day, Ket, Kit Kat, Mauve, Purple, Rockmesc, Special K, Special LA Coke, Super Acid, Super C, Super K, and Vitamin K
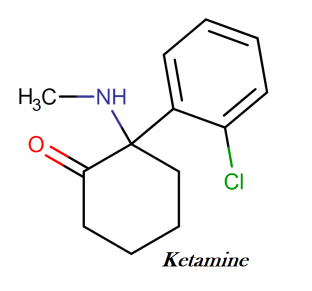
Ketamine IUPAC name, chemical structure, mass, formula
IUPAC name: 2-(2-chlorophenyl)-2-(methylamino)cyclohexan-1-one
Other (trade) names: γ-Hydroxybutyric acid, G, Sodium Oxybate
Molecular formula: C13H16ClNO
Molecular weight: 237.725 g/mol
Molecular structure:
Ketamine drug class
This compound belongs to the class of organic compounds known as chlorobenzenes. These are compounds containing one or more chlorine atoms attached to a benzene moiety.
Ketamine chemistry and racemic composition
Ketamine is a chiral molecule that is available in commercial preparations as a racemic mixture of equal amounts of R (−) – ketamine and S (+) ketamine enantiomers. The latter enantiomer is about 2 – 4 times a more potent analgesic than R(−) enantiomer, but the R(−) – enantiomer may contribute to the emergence reactions associated with ketamine anesthesia.
In mice, the hypnotic effect of the S (+) – ketamine isomer is approximately 1.5 times greater than the R (−) – ketamine isomer. Ketamine is a high lipid soluble weakly basic amino compound that usually occurs in pharmaceutic preparations as the hydrochloride salt.
Ketamine history of use
Calvin Stevens synthesized ketamine hydrochloride at the Park- Davis Laboratories in 1962. Early clinical studies suggested that ketamine was an effective anesthetic agent with less toxicity, little respiratory depression at anesthetic doses, and fewer emergence reactions than phencyclidine.
During the late 1960s, ketamine was marketed as the dissociative anesthetic, under the name Ketalar and was used to treat soldiers in the Vietnam War. The abuse potential of ketamine was recognized in the early 1970s, but reports of ketamine abuse in human and veterinary medicine did not appear until the early 1980s in Australia and in the early 1990s in the United States
Ketamine legal status
In the United States, ketamine is a Drug Enforcement Agency (DEA) schedule III substance (drugs with currently accepted medical indications and abuse potential for low to moderate physical dependence or high psychologic dependence).
How does ketamine look like? How is ketamine abused?
The usual form of ketamine is a liquid, but evaporation of this liquid crystalizes ketamine. The crystal residue is ground into a powder, similar in appearance to cocaine or heroin.
Like phencyclidine, ketamine is smoked as a cigarette after the addition of ketamine to tobacco or marijuana. Because of the diffi culty manufacturing ketamine clandestinely, illicit ketamine is usually a pharmaceutic preparation diverted from legal stocks, particularly from veterinarian clinics. Although ketamine is occasionally an adulterant of heroin, illicit stocks of ketamine are usually relatively pure.
Ketamine mechanism of action
Ketamine is a dissociative anesthetic with analgesic and amnestic properties that causes impairment of working and episodic memory during intoxication and the immediate period after the administration of ketamine.
Similar to phencyclidine (PCP), ketamine is a noncompetitive antagonist of the NMDA receptor for glutamate, but the mechanism of action of ketamine is more complex than PCP because of the interaction of ketamine with many others receptors (opioid, noradrenaline, serotonin, muscarinic cholinergic).
These effects also include decreased catecholamine reuptake and the stereoselective inhibition of the dopamine transporter with the S(+) – enantiomer being approximately 8 times more potent than the R(−) enantiomer. The affinity of PCP for the NMDA receptor is approximately 10-fold greater than ketamine.
The administration of subanesthetic doses of ketamine to schizophrenic individuals produces short-term activation of psychotic symptoms, which are similar to their usual psychotic episodes.
Following anesthetic doses (> 2 mg/kg), ketamine produces a dose-related increase in heart rate and pressure without altering stroke index. Ketamine does not cause significant respiratory depression except following very large doses or rapid IV administration.
Ketamine medical uses
Third World physicians report that ketamine is safe for surgical use outside high-tech environments. It is given as a pain reliever and, less commonly, to reduce convulsions. Ketamine is also a veterinary anesthesia drug used with wild animals ranging from giraffes and gazelles to polar bears and arctic foxes. Success has also been reported with using ketamine to supplement alcoholism therapy.
Two researchers reported that ketamine therapy with 42 alcoholics produced a two-year abstinence from drinking in 15 of them, an outstanding result. Such results have prompted researchers to speculate that ketamine may also be useful in treating addiction to drugs other than alcohol.
Experiments indicate that ketamine may have the potential for treating migraine headache and depression, and researchers have seen evidence that ketamine may improve asthma and shrink breast cancer cells. Ketamine can reduce phantom limb pain, a strange affliction in which a person senses that an amputated limb is still present and hurting.
The drug has been used in psychotherapy to help persons face and deal with unpleasant memories, a process accompanied by what researchers described as “mind expanding effects.” Ketamine has also been investigated as a potential defense against the chemical warfare agents soman and diisopropylphosphorofluoridate.
Healthy volunteers receiving ketamine in an experiment have experienced sensations reminiscent of LSD. Researchers have described such effects as “profound” among alcoholics, and illicit ketamine users have said such effects are “intense.” The substance can prompt people to feel like they are becoming transparent, blending into nearby individuals, or becoming an animal or object.
Users may feel like their bodies are transforming into harder or softer substances. Persons may think they remember experiences from a past life. Some users take the drug to enter the “K-hole,” a semi-paralytic state described as similar to near-death experiences in which people perceive their consciousness as floating above their bodies, sometimes accompanied by meaningful hallucinations and by insights about the user’s life and its proper place in the cosmos.
Ketamine dose-effect
Illicit use:
Recreational doses are highly variable (50 – 200 mg), in part, because of the rapid development of tolerance to ketamine. Typical illicit doses of ketamine are 25 – 50 mg intramuscularly, 30 – 75 mg insufflation, and 75 – 3 00 mg orally. The intense, dissociative experience persists approximately 1 hour. Case reports document the daily use of up to 4 – 7 g ketamine. Insufflating 30 – 50 mg ketamine (i.e., a small line) produces a dreamy state, whereas the intramuscular administration of 60 – 125 mg results in a more intense dissociative state (“K – hole”).
Medical use:
Ketamine is a rapidly acting, relatively safe anesthetic agent that is a common agent for conscious sedation in children. The bronchodilating properties are useful for the sedation of asthmatic patients requiring intubation.
The typical anesthetic dose of ketamine for conscious sedation is 1 – 2 mg/kg intravenously or 4 – 5 mg/kg intramuscularly. Experimental uses of ketamine include the use of low-dose ketamine for postoperative pain relief for regional or local anaesthesia, and for opioid-sparing effects. The emergence reaction after ketamine administration is not dose-dependent.
Ketamine effects
A case report tells of recreational users experiencing temporary paralysis. Nausea and vomiting have been reported, and scientific literature contains several mentions of temporary breathing interruption caused by the drug. Increased pressure within the eye (a potential problem for glaucoma sufferers) has been measured following a ketamine dose, but not all researchers looking for that effect have found it.
The drug can interfere with a male’s physical ability to engage in sexual activity. Experiments show that ketamine can cause brain damage in rats and that simultaneous use of nitrous oxide worsens the damaging action. Ketamine can cause nervous agitation, extra salivation, blood pressure elevation, abnormal heartbeat, and muscle injury. Persons suffering from the body chemistry disorder porphyria should exercise caution about ketamine use.
The drug can change perceptions of one’s surroundings. Tests indicate ketamine can alter visual perception for at least 24 hours, causing people to misjudge size and speed of objects (implying that driving skills may be impaired). Long-term use may cause persistent difficulties with attention, memory, and learning ability. The substance can create amnesia about what happens while a person is under the drug’s influence.
Ketamine’s psychological actions have been characterized as similar to temporary schizophrenia. A study examining persons who received the drug during surgery found that upon awakening some felt they were floating; some were euphoric; some screamed in apparent terror. A study found such effects to be twice as common in female patients as in males. Such effects are stronger among alcohol abusers.
The floating sensation may occur as people regain consciousness before they regain sense of touch, a sequence that would temporarily eliminate awareness of gravity. One surgery patient experienced LSD like effects that continued even after release from the hospital. Reports exist of patients experiencing psychological effects for a year after a dose.
A reviewer who examined many years of scientific reports about ketamine, however, found a consensus that long-term psychological consequences from ketamine occur no more frequently than with other anesthetics-a conclusion about incidental effects from anesthetic use, not about deliberate effects induced as part of psychotherapy or illicit use.
One authority claims that the greatest physical hazard has a psychological base, as users sometimes become indifferent about death and take risks they would otherwise avoid. Persons intoxicated with ketamine may be woozy and have lower perception of pain, conditions that can cause or worsen accidents. Female lemmings are more susceptible to the drug than males.
While the male-female difference does not necessarily carry over to humans, use of ketamine’s anesthetic properties by sexual predators seeking to weaken victims was publicized in the 1990s. Researchers using the drug to treat alcoholism have found that ketamine makes a person more susceptible to suggestions, perhaps making a person more vulnerable to manipulation.
Ketamine side effects
Ketamine is generally safe for those critically ill when administered by trained medical professionals. Even in these cases, there are known side effects that include one or more of the following:
- Cardiovascular: abnormal heart rhythms, slow heart rate or fast heart rate, high blood pressure or low blood pressure
- CNS: Ketamine is traditionally avoided in people with or at risk of intracranial hypertension(ICP) due to concerns about ketamine causing increased intracranial pressure. It does not increase ICP more than opioids.
- Dermatologic: Transient reddening of the skin, transient measles-like rash
- GIT: reduced appetite, nausea, increased salivation, vomiting
- Local side effects: Pain, eruptions or rashes at the injection site
- Neuromuscular and skeletal: Increased skeletal muscle tone (tonic-clonic movements)
- Ocular side effects: Double vision, increased intraocular pressure, involuntary eye movements, tunnel vision
- Respiratory side effects: Airway obstruction, cessation of breathing, increased bronchial secretions, reduced effort to breathe, spasm of the vocal cords (larynx)
- Other: Anaphylaxis, dependence, emergence reaction
At anesthetic doses, 10–20% of people experience adverse reactions that occur during emergence from anesthesia, reactions that can manifest as seriously as hallucinations and delirium.
These reactions may be less common in some people subpopulations, and when administered intramuscularly, and can occur up to 24 hours postoperatively; the chance of this occurring can be reduced by minimizing stimulation to the person during recovery and pretreating with a benzodiazepine, alongside a lower dose of ketamine.
People who experience severe reactions may require treatment with a small dose of a short- or ultrashort-acting barbiturate. Tonic-clonic movements are reported at higher anesthetic doses in greater than 10% of people.
Ketamine overdose
There are relatively few cases of ketamine overdose reported in the medical literature, primarily involving inadvertent administration of excessive ketamine doses to children undergoing sedation or anesthesia. In these patients, the main complications are transient respiratory depression and prolonged sedation up to 24 hours.
Fatalities associated with ketamine are usually related to either behavioral-induced trauma or multiple-drug overdose. In a series of 15 nonhospital- associated deaths with detectable postmortem concentrations of ketamine, 12 involved multiple drugs and 2 involved trauma. The other death resulted from natural causes (sarcoidosis).
Ketamine abuse
Desired effects associated with ketamine use may include euphoria, depersonalization, derealization, universal empathy, sudden insights into the nature of existence or oneself, and perceptual distortions (sounds, shapes, colorful visions, floating feeling, the absence of time, body image). The “ K – hole ” refers to the development of tunnel vision during intoxication followed by the feeling of rising above the body like a near-death experience.
Although some individuals experience recurrent psychoses following repeated binges on ketamine, there is insufficient evidence to support the development of sensitization to the behavioral effects of ketamine.
Who abuses ketamine the most?
Ketamine came on the recreational drug scene in the early to mid 1980s. It became part of the nightclub scene and also was popular in certain dance cultures, including raves, originally to increase the effects of MDMA (ecstasy).
Even after it was given the Schedule III classification in 1999, recreational use has continued to grow since then. It remains a party drug, often used by high school students and young adults in order to achieve a hallucinatory, dream-like state.
Ketamine has also a high potential for abuse among people who are attempting to self-medicate depression or suicidal ideation due to its ability to so quickly alleviate these states. Psychiatrists are even studying the potential of ketamine to be used as an immediate remedy for suicidal urges and deep depression.
A patient could come into a hospital feeling suicidal and be rapidly lifted out of that state of depression and despair with a controlled dose of ketamine. Once that person is feeling better, the root cause of those feelings could be effectively addressed, and an outpatient program of therapy, long-term medication options, and other treatments could be planned.
Ketamine addiction
Although the high caused after ketamine use is extremely pleasant, it can lead to serious dependence. Ketamine has the potential to lead to tolerance and addiction. Once an addiction develops and an individual is using the drug most of the time, it can become easy to spot since its effects on the state of mind are so intense.
Signs of a ketamine addiction may include:
- Frequent state of distraction and/or drowsiness
- Fatigue or lack of motivation
- Difficulty concentrating
- Reduced ability to feel physical pain
- Slurred speech
- Redness of the skin
- Loss of coordination
- Insomnia
- Bladder pain
- Incontinence
Ketamine abstinence syndrome
Case reports of abstinence following chronic ketamine abuse associated the development of intense drug craving, anxiety, fatigue, diaphoresis, and tremulousness within 8 hours after cessation of use. Within 24 – 48 hours after ketamine use ceases, lethargy, depression, and anorexia occur. After a period of deep sleep, the individual feels better with some residual weakness.
Ketamine withdrawal
Ketamine withdrawal occurs when a user has taken excessive amounts of Ketamine, either for a long time or many times over and then tries to quit. The body has adjusted to life with the drug and when the user takes the drug away, a range of side effects arise such as paranoia, depression, emotional imbalance and physical imbalance. These symptoms are the result of the withdrawal that is taking place from the lack of Ketamine in the daily routine.
Although the majority of ketamine withdrawal symptoms are not physical in nature, they still make it difficult for the average user who is addicted to the drug to simply “throw in the towel” and quit using ketamine abruptly. Symptoms of withdrawal can make it difficult to remain sober and cravings may lead the user right back to his or her previous behavior of drug abuse.
Unfortunately, the only way for the symptoms of ketamine withdrawal to go away is for the user to remain abstinent from the drug and allow the symptoms to run their course or to use the drug and then start the process all over again.
Common symptoms include:
- Double vision
- Hearing loss
- Increased heart beat
- Rapid breathing
- Loss of motor skills
- Loss of coordination
- Depression
Ketamine absorption, metabolism and excretion
After IV administration, ketamine is rapidly absorbed and plasma concentrations peak at around 0.75 g/ml approximately 1 hour post-administration.
An estimated 20% to 50% of ketamine binds to plasma proteins and is distributed at a volume of 1 to 3 L/kg throughout the body. High concentrations of ketamine are thought to appear within fat stores, the liver, lungs, and brain – whereas low concentrations appear within heart, muscle tissue, and plasma.
After administration, ketamine is subject to extensive hepatic metabolism via various CYP450 isoenzymes including CYP3A4, CYP2B6, and CYP2C9. CYP3A4 facilitates a majority of the metabolism via N-demethylation to form the pharmacologically active metabolite “norketamine” – which has approximately 16% the potency of ketamine. Norketamine is subject to additional dehydrogenation to form the secondary metabolite, dehydronorketamine.
Additional hydroxylation of the cyclohexone ring, conjugation with glucuronic acid, and dehydration of hydroxylated metabolites occurs prior to urinary excretion. Ketamine is thought to be eliminated from the system in a biphasic or triphasic pattern. The initial phase of elimination is thought to exhibit a 15 minute elimination half-life, whereas the secondary phase of elimination may occur between 2 and 4 hours post-administration.
This indicates that it could take up to 22 hours for complete plasma elimination of ketamine, but most likely will take just under 14 hours (on average). An estimated 90% of ketamine is processed by the kidneys and excreted via urine, whereas 3-5% is excreted via feces. Of the 90-95% that is eliminated via urine, only 2-4% is of unchanged ketamine – the majority is of metabolites such as norketamine and dehydronorketamine.
How long ketamine stay in your system?
The elimination half-life time of ketamine is reportedly 2.5 to 3 h in adults and 1 to 2 h in children, meaning that those who are healthy adult, they will eliminated ketamine from their plasma on average between 13 hours 45 minutes and 16 hours 30 minutes.
Ketamine is metabolized to form metabolites such as norketamine and dehydronorketamine, but these metabolites are known to exhibit shorter elimination half-life times than ketamine. Most users can expect to have excreted a majority of the drug within 24 hours of their last dosage, and completely from their body within several days thereafter.
Ketamine drug interactions
In surgery patients administering diazepam simultaneously with ketamine has diminished unwanted psychological effects such as delirium and nightmares. Midazolam may also help. In experimentation with rats and mice the actions of ketamine and alcohol have similarities, and the two have cross-tolerance (meaning one can substitute for the other in various ways).
Human alcoholics report that ketamine produces sensations like those of alcohol. A small study found that ketamine has stronger effects on perceptions and thinking skills in alcoholics than in other persons. In rats, morphine can boost some pain relief from ketamine, and ketamine can reduce pain relief from morphine.
In contrast, a human experiment found that patients needed less morphine for pain relief if they also received ketamine. In humans, ketamine can boost opiate and barbiturate actions so much as to be fatal. Lorazepam can boost the sedative and amnesia qualities of ketamine in humans.
Ketamine intoxication treatment
Treatment is supportive with careful attention to the evaluation and treatment of any cardiorespiratory dysfunction. Symptoms are typically brief with most patients discharged from the emergency department within 5 hours of presentation.
The failure of symptoms to ameliorate after 2 hours of observations suggests another drug or disease process, particularly if seizures, hemodynamic changes, or hyperthermia are present. The most serious adverse effects of ketamine intoxication are respiratory depression, agitation, and rhabdomyolysis. Patients should be placed in a quiet environment with minimal external stimulation.
Are there some antidotes for ketamine intoxication?
There are no specific antidotes. The treatment of emergence reactions primarily involves the use of benzodiazepines (e.g., adults: lorazepam 1– 2 mg, IV, titrated to effect). Preliminary clinical studies suggest that haloperidol (5 mg IM, repeated in 30 minutes if needed) is an alternative to benzodiazepines. However, there are inadequate data to assess the safety or efficacy of haloperidol in this setting.
Can commercial drug tests detect ketamine?
Unless there is a particular reason to be looking for it, as in the case of an autopsy, specific ketamine tests are not normally conducted. It is not one of the SAMHSA-5 standardly tested for in the basic drug test, nor is it included in the extended drug tests. a ketamine-specific test is well equipped to detect norketamine and dehydronorketamine metabolites.
However, as of 2013, extended panel lab tests are now including ketamine in some areas.
Ketamine detection in urine, blood, saliva and hair
Urine tests: The most common type of test to determine whether someone has ingested ketamine is via collection of a fresh urine sample. The sample is then sent to a laboratory for a urinalysis which reports levels of various metabolites such as norketamine and dehydronorketamine. Since urinary excretion of unchanged ketamine is relatively low, ketamine isn’t generally a preferred biomarker on urinalyses.
By utilizing techniques such as gas chromatography/mass spectrometry (GC/MS), it is possible to detect norketamine within a urine sample for up to 14 days after ketamine administration. Research in monkeys found that norketamine could remain detectable for up to 31 days after ketamine administration. Detection limits are generally set at 5ng/mL, making the metabolites detectable among heavy users for 1-2 weeks after their last dose.
Hair tests: It is possible to detect ketamine by collecting a sample of hair follicles from a prospective user’s head. The sample of hair follicles can then be sent to a laboratory for analysis, which will determine levels of ketamine and its metabolite norketamine (and sometimes dehydronorketamine).
Researchers have proposed that these tests should utilize a cutoff threshold of 0.5 ng/mg for ketamine and 0.1 ng/mg norketamine in a hair sample; concentrations above these limits indicate repeated exposure to ketamine.
Hair tests may be advantageous over urine tests in that they may provide a longer window of detection of up to several months after ketamine ingestion. One study determined that the amount of ketamine within hair samples correlates directly to the frequency of use/abuse. Concentrations of ketamine and norketamine are easiest to detect in hair, whereas the metabolite dehydronorketamine is only likely to appear among high dose users.
Saliva tests: Oral fluid (saliva) samples can be collected to determine whether an individual has recently ingested ketamine. Various devices such as the OratectXP Oral Fluid Drug Screen Device are being engineered to rapidly detect ketamine in an oral fluid sample. It is thought that these devices would be useful for law enforcement agents to pinpoint the specific drug responsible for an individual’s intoxication.
The cutoff for ketamine detection in oral fluid devices like the OratectXP is set at 15 ng/ml. Currently the accuracy of such devices are approximately 94%, and as a result, they may be utilized more often in the future – especially as accuracy increases at lower thresholds.
Furthermore, collection of an oral fluid sample and analysis in a laboratory via liquid chromatography/mass spectrometry (LC/MS) is highly accurate – and may be used to confirm results from a device like the OratectXP. That said, ketamine is unlikely to remain in your saliva for an extensive term after administration.
For this reason, it is likely that saliva tests would be reserved for assessing intoxication solely on the day of intoxication – rather than several days thereafter.
Blood tests: A blood test is seldom utilized to determine levels of ketamine due to the fact that it is invasive and offers a smaller window of detection compared to urine tests. For this reason, most individuals subject to a ketamine test will be assessed with a urine sample. Ketamine is thought to get eliminated from the plasma within 24 hours of administration.
As a result of this fast elimination, it remains difficult to detect via collection of a blood sample. A blood test may be utilized in scientific research to confirm plasma concentrations of the drug and/or among hospitalized patients. Additionally, a blood test is effective when collected the day of ketamine administration, but detectability of ketamine (and metabolites) in the bloodstream diminishes with each passing day.