Contents
- What is angular cheilitis?
- What are different medical terms for angular cheilitis?
- Is angular cheilitis contagious?
- Angular cheilitis symptoms
- What are the different types of angular cheilitis?
- Can angular cheilitis become chronic?
- What are the causes of angular cheilitis?
- Weak immune system and angular cheilitis
- Candida infection as a cause of angular cheilitis
- Bacterial infection as a cause of angular cheilitis
- Vitamin B2 (riboflavin) defficiency and angular cheilitis
- Iron defficiency and angular cheilitis
- Zinc deficiency and angular cheilitis
- Contact dermatitis as a cause of angular cheilitis
- What “bad habits” may cause angular cheilitis?
- What underlying conditions may be related with angular cheilitis?
- What drugs may cause angular cheilitis?
- Angular cheilitis diagnosis
- Angular cheilitis vs Cold sores
- Angular cheilitis treatment options
- Topical corticosteroids for angular cheilitis
- Do antibiotics work well for angular cheilitis?
- Can OTC clotrimazole cream cure my angular cheilitis?
- Miconazole for angular cheilitis
- Lamisil for angular cheilitis
- Tinactin for angular cheilitis
- Zinc Oxide paste for angular chelitis
- Angular cheilitis in children
- Angular cheilitis during pregnancy
- Anglular cheilitis in elderly
- Can angular cheilitis cause scars?
- What should I avoid if I have angular cheilitis?
- Can Vitamin B complex supplements heal my angular cheilitis?
- Is Carmex effective for angular cheilitis?
- Is Candex effective for angular cheilitis?
- Is Blistex helpful for angular cheilitis?
- What natural moisturizers can I use for my angular cheilitis?
- Can sun, saltwater and chlorine cure my angular cheilitis?
- What natural remedies can I use for my angular cheilitis?
- Water and angular cheilitis
- Baker soda and angular cheilitis
- Lemon and angular cheilitis
- Cucumber and angular cheilitis
- Tea tree oil and angular cheilitis
- Aloe Vera and angular cheilitis
- Honey and angular cheilitis
- Margosa leaves and angular cheilitis
- Yoghurt and angular cheilitis
- Listerine and angular cheilitis
- Active oxygen and angular cheilitis
- What diet changes should I make for angular cheilitis?
What is angular cheilitis?
Angular cheilitis or angular stomatitis is an inflammatory condition localized on one or both corners of the lips characterized with redness, swelling, and irritated skin that breakdown and crust. It can also be painful and itchy. It is most commonly bacterial or fungal infection or mixed bacterial/fungal infection, however, other factors may also lead to this condition.
Angular cheilitis most commonly occur in immunocompromised patients, atopic patients and patients with nickel allergy. Patients older than 30 years are most commonly affected. It can last from few days to years.
What are different medical terms for angular cheilitis?
Angular cheilitis is also known as:
- Perleche
- Angular stomatitis
- Corner of mouth sores
- Cracked lip corners
- Sores on corner of lips
- Sores on mouth corners
Is angular cheilitis contagious?
Angular cheilitis is not contagious. Many will think that it is contagious because it can be caused by bacteria or fungal infection or because it looks similar to other contagious mouth diseases such as cold sores and fever blisters, but it should be known that it is not the case for angular cheilitis.
Angular cheilitis symptoms
The main signs and symptoms of angular cheilitis that patient may notice are irritation and soreness in one or both corners of the lips. Other signs and symptoms that can be noticed on the skin are:
- Bleeding
- Blistering
- Cracked skin
- Crusty skin
- Itching
- Pain
- Redness
- Scaly lips
- Swelling of the lips
A lot of causes may lead to this condition, therefore the appearance of the lesion may be different from person to person. Lesions are usually symmetrical localized on both sides of the mouth, but in some cases only one side may be affected.
The lesion may be sometimes limited only to the mucosa of the lips, and in other situations it may spread past the edge where the lining on the lips becomes the skin also known as the vermilion border.
Initially, the corners of the mouth develop a gray-white thickening and redness. Later, appearance starts to look like erythema triangular area with swelling and the skin being breakdown at either corner of the mouth.
The mucosa of the lip may become cracked, ulcerated, ulcerated or atrophied. Bleeding is usually not observable. If Staphylococcus aureus bacteria are involved, the lesion may show golden yellow crusts. Rarely, the dermatitis can extend from the corner of the lips even to to the skin of the cheek or chin.
If cheilitis is caused by nutritional deficiency of an underlying the condition, different other signs and symptoms may be recognized, such as glossitis or swollen tongue. Those with angular cheilitis who wear dentures, erythematous mucosa underneath the denture might appear consistent with denture-related stomatitis
What are the different types of angular cheilitis?
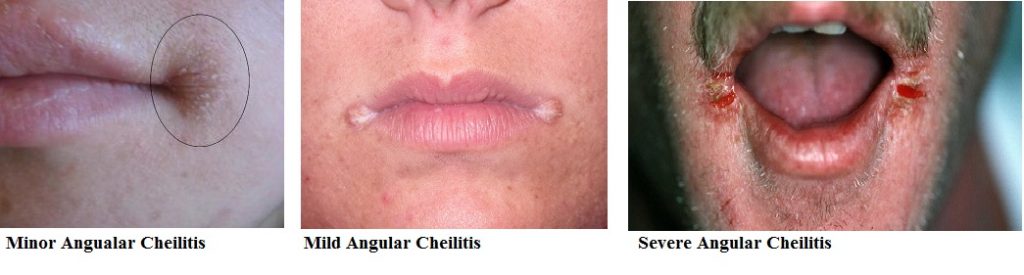
Depending on severity angular cheilitis can be divided in 3 groups:
Minor angular cheilitis
These symptoms of minor angular cheilitis will generally go unnoticed. Following symptoms are:
- Tightness in one or both corners of the lips
- Small flaky skin in the corners of the lips
- Slight discomfort when opening when mouth are open wide
Mild angular cheilitis
The usual discomforts that may be noticed in the case of mild form of this condition are:
- Noticeable discomfort in both or one corner of the mouth opening the mouth wide, or when eating
- Buildup of dry and flaky skin in one or both corners of the mouth
- Slight redness with or without swelling in the corner of mouth
Severe angular cheilitis
In some cases, many patients will misdiagnose this form of angular cheilitis with a cold sore. In most cases OTC ointments wouldn’t be helpful to treat the issue. Severe angular cheilitis may cause significant discomforts during talking, eating, opening and closing the mouth. Other signs and symptoms may include:
- Noticeable blisters at one or both corners of your mouth.
- Split corners at the edges of the mouth which do not heal.
Can angular cheilitis become chronic?
Yes, angular cheilitis can become chronic, especially if it is not treated properly. Angular cheilitis can last for few or more months or even years. It can be also recurrent condition. Chronic angular cheilitis is most common in individuals who have have a weakened immune system, high stress lives or drool in their sleep.
What are the causes of angular cheilitis?
The etiology of angular chelitis is complex and it is considered as multifactorial disorder. Bacterial or fungal infection, Vitamin-B2 and iron deficiency or atopia are most common causes of this condition. So, causes of angular cheilitis may be:
- Bacterial infection
- Candida infection
- Polymycrobial infection or mixed bacterial/fungal infection
- Angular herpes simplex
- Vitamin B2 (riboflavin) deficiency
- Vitamin B5, B12, B3 or folic acid deficiency
- Iron and Zinc deficiencies
- Hormonal imbalances
- Bad weather conditions
- Irritation of the skin caused by makeup cosmetics, lipsticks or balms, mouthwashes, toothpastes, etc.
- Contact dermatitis or other allergy
- Alcoholism
- Celiac disease
- Dehydration and not drinking enough water
- Mouth breathing that creates a continuous air flow around the mouth leading to dry lips
- Poor Habits like licking or biting the lips
- Smoking ciggaretes.
- Systemic disorders
- Drugs
Weak immune system and angular cheilitis
Our bodies hold a host of bacteria, fungus and viruses at all times, and the mouth is no exception. However the body may lose the balance when the immune system gets compromised.
As such, the same “good” bacteria and viruses may turn to be pathogenic and may cause various issues in the body. Once the immune system gets weak, the bacteria from saliva may lose the balance and cause conditions like the angular cheilitis.
The angular cheilitis is also usual symptom in a HIV infected patients. Stress could be also another risk factor to the body and may weaken immune system. Patients suffering from diabetes, and who those who are taking antibiotics or corticosteroids drug for a long-term are all likely to get the angular cheilitis.
Candida infection as a cause of angular cheilitis
20% of all angular cheilitis are caused by Candida albicans infection. In approximately 93% of angular cheilitis lesions Candida can be isolated. This yeast is normally detectable in the mouths of about 40% of healthy individuals, as a normal component of the oral microbiota. However, Candida is known to show dimorphism.
First form is yeast that is known to be relatively harmless and also beneficial in the body and the second is a pathogenic hyphal form which is related with invasion of host tissues. Usually people get angular cheilitis from Candida infection when their body immunity gets compromised.
In some individuals the mouth may act as a Candida reservoir reinfecting the sores at the corners of the mouth and preventing the sores from healing. Potassium hydroxide preparation is generally recommended to help distinguish between mentioned two forms, and thus highlight which cases of angular cheilitis are caused by Candida.
Angular cheilitis secondary caused by Candida albicans infection should be treated with topical antifungal creams. However in patients with HIV given topical therapy for angular cheilitis, relapses occur more frequently than in those treated with systemic antifungal therapy.
Bacterial infection as a cause of angular cheilitis
In about 20% of cases with angular cheilitis, Staphylococcus aureus infection can be the major cause. β-hemolytic streptococci infection has been also detected in between 8–15% of cases of angular cheilitis but less commonly are present in isolation.
The proposed mechanism of causing bacterial angular cheilitis is bacterial transfer from the anterior nares to the mouth angles probably through the respiratory infection and because of increased nasal secretion.
Conditions that may cause bacteria spreading include:
- Touching your lips with dirty fingers
- Having chapped lips
- Chewing on your fingernails
- Chewing on objects that carry germs
When Staphylococcus aureus is involved, topical treatment with a coadministration of mupirocin or fusidic acid and 1% hydrocortisone cream proves to be effective treatment. Topical preparations should be applied at the angles of the mouth and at the anterior nares if the area is found to be colonized.
Vitamin B2 (riboflavin) defficiency and angular cheilitis
Vitamin B2 is needed for proper metabolism of fats and it also works as an antioxidant, destroying the oxygen-free radicals which can damage the cells and their DNA. It is also needed for collagen synthesis.
Patients with Vitamin B2 deficiency or ariboflavinosis, usually have a deficiency in the other B vitamins as well. Defficency may happen due to malnutrition or malabsorption of the nutrients. Such defficiency may lead to cheilitis.
The proposed mechanism in which vitamin B2 deficiency may lead to angular cheilitis is reduced activity of the enzyme lysyl oxidase which affects the formation of collagen cross-linking.
Such interruption may be important cause of skin damage. Vitamin B2 deficiency may also cause other conditions such as redness of mucous membranes, and colored glossitis.
Iron defficiency and angular cheilitis
Iron has many important functions in human organism. However, it is not completely understood how iron deficiency may cause angular cheilitis, but it is known that reduced levels in blood may decrease efficiency of the immune system and anemia which may in turn allow an opportunistic infection of candida or herpes simplex.
Zinc deficiency and angular cheilitis
Zinc is an important mineral for proper function of immune system and many other functions in the body. Patients with zinc deficiencies are more susceptible to the infections that may be the causes of angular cheilitis.
Contact dermatitis as a cause of angular cheilitis
In almost ¼ of cases of angular cheilitis is caused by irritants. As saliva contains digestive enzymes, it may exhibit some digestive action on face tissues if they are in contact frequently.
The mouth corners are regularly exposed to saliva usually more than any other part of the lips. Angular cheilitis is more commonly seen in people without any teeth, because their salivation is increased.
Angular cheilitis is also commonly observable in persons with denture wearers. It is also present in about 30% of patients with denture-associated stomatitis. Ultraviolet light exposure and smoking are also common causes of angular cheilitis.
Potential allergens may be present in some types of toothpaste, lipstick, acne products, cosmetic products, chewing gum, mouthwash, foods, dentures or mercury containing amalgam fillings. These allergens may cause allergic dermatitis if they get in contact with the skin, provoking angular cheilitis.
The sunscreen that can be found in some types of lip balm will degrade over time into an irritant. Such irritants can initiate mild angular cheilitis, and when the person applies more lipbalm in order to alleviate the cracking, it will only aggravate it.
What “bad habits” may cause angular cheilitis?
Bad habits that keep the mouth corners constantly moist such as: chronic lip licking, sucking objects such as pens, lollipops, thumb sucking, flossing, chewing gum, drooling and mouth breathing may cause angular cheilitis. Terms such as perlèche (comes from French word pourlècher meaning “to lick one’s lips”), or “factitious cheilitis” are applies to this cause.
The medical term “cheilocandidiasis” describes exfoliative lesions around the lips caused by a superficial candidal infection due to chronic lip licking. Some individuals may lick their lips in order to provide a temporary relief, only serving to worsen the condition.
Different underlying conditions may be involved in angular cheilitis. Most commonly such conditions lead to weak immunity, or malabsorption of essential nutrients and thus their deficiency which may lead to cheilitis. Following conditions may be the cause of angular cheilitis:
- Anorexia nervosa – due to malaborption of essential nutrients and weaken immunity
- Orofacial granulomatosis – due to altering of the local anatomy and extenuating the skin folds at the corners of the mouth
- Xerostomia (dry mouth) – 5% of cases of angular cheilitis
- Sialorrhoea – due to excessive salivation and creating a constant wet environment in the corners of the mouth
- Down syndrome – due to relative macroglossia. Patients with this syndrome are known to have an apparently large tongue in a small mouth, which may constantly stick out of the mouth causing soaking of the corners of the mouth with saliva. In almost 25% patients with Down syndrome, angular cheilitis is observable.
- Inflammatory bowel diseases including Crohn’s disease or ulcerative colitis – due to malabsorption and nutrients loss via diarrhea, but also because of immunosuppressive therapy that may cause angular cheilitis.
- Glucagonomas (pancreatic tumors) – due to hypersecretion of glucagon that may cause dermatitis. Angular cheilitis is very common in patients with glucagonomas
- Oropharyngeal, esophageal or mucocutanous candidiasis
- HIV infection
- Diabetes
- Neutropenia
- Eczema
- Sideropenic dysphagia
- Plasma cell ginigivitis
- Melkersson-Rosenthal syndrome
What drugs may cause angular cheilitis?
In some cases angular cheilitis may be caused by drugs. Isotretionin is an analog of vitamin A that may dry the skin. Other drugs that commonly cause angular cheilitis are indinvair and sorafenib. Hypervitaminosis of Vitamin A has been also shown to cause this condition. Corticosteroids are immunosuppressive agents that may also provoke indirectly by causing oropharingeal candidiasis.
Some recreational drugs abusers may also develop angular cheilitis. Examples include methamphetamines, cocaine, heroin, and hallucinogens users.
Angular cheilitis diagnosis
Physical examination is sometimes sufficient indicator for angular cheilitis diagnosis. Typically both corners of the lips are affected. Initial lesions are small, grey-white color thickened areas bordered by mild erythema while established lesions exhibit a blue-white shade and are linked with scaling, and patches around the skin.
Severe forms have visible maceration, fissuring and crusting. Physical examination may also discover evidence of lip licking, chewing, drooling, or present predisposition such as dental malocclusion or bad fitting dentures.
Presence of fungal and bacterial lesions and its identification may be helpful in choosing appropriate therapy, since angular cheilitis has been related with infective organisms including Candida albicans, Staphylococcus and Streptococcus spp, and rarely gram negative species. Skin biopsy is not necessary for this diagnosis.
Nutritional deficiency of iron, vitamin B2, folate, vitamin B12 or zinc can be also causes of this condition. Anemia or hypervitaminosis of vitamin A may also be predisposed factors.
Thus, it is very important to identify underlying condition, because by managing them, angular cheilitis will be also cured. In that case, laboratory testing should be considered and complete blood cell and reticulocyte count, vitamin, iron and zinc levels should be measured.
The differential diagnosis of angular cheilitis includes physical trauma, chemical injury, and allergic contact dermatitis.
Angular cheilitis vs Cold sores
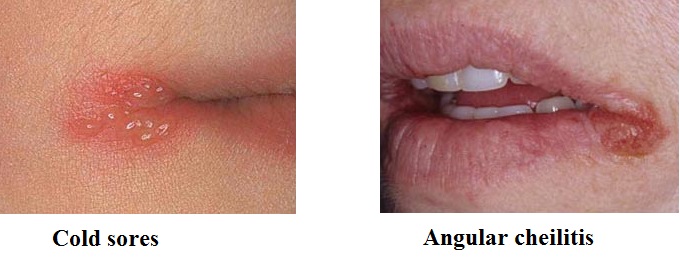
Angular cheilitis manifestation seems similar to many other mouth conditions, which may lead to people to incorrectly diagnose it and because of this use the wrong treatments. The main difference between cold sores and angular cheilitis is that cold sores are caused Herpes Simplex Virus infection while angular cheilitis is mostly bacterial/fungal infection. Cold sores are usually healed within 2-3 weeks while angular cheilitis last longer.
The signs and symptoms of cold sores begin with tingling and itchy sensation that will then turn into a red area forming one or many small blisters. Eventually these small blisters will produce a large red blister which will then swell until it erupts creating a weeping ulcer.
Angular cheilitis starts as dry flaky skin that turns into a red welt then if untreated progressively gets worse and making your lips corners to split leaving open wounds. Another important difference is that cold sores appear mostly on the lips while angular cheilitis is localized only on the corners of the mouth. The difference can be seen on picture below:
Angular cheilitis treatment options
After detailed physical examination and/or laboratory analysis it can be determined if the cause has mechanical, nutrtitional, bacterial and/or fungal origin or if angular cheilitis is caused by underlying condition.
Treatment options for angular cheilitis are: medical, surgical or behavioral management.
Medical treatment of angular cheilitis
Medical treatment may include:
- Supplementation of nutritional deficiencies. Supplementation with vitamin B2, B12, folic acid, iron, zinc, etc..
- Topical anti-fungal agent (clotrimazole, ketoconazole, miconazole, nystatin) in combination with barrier paste (zinc oxide) and topical corticosteroid with low to mid-potency.
- Topical antibiotic such as mupirocin, clindamycin or erythromycin if bacterial culture is positive or if there is suspicion for bacterial infection
- Administration of barrier paste (zinc oxide) or emollient (petrolatum, lip balm) for barrier protection
- Monotherapy with topical corticosteroids of low to mid potency
- Intralesional corticosteroid administration
One small study showed that treatment with topical nystatin was effective and shortened time of cheilitis healing compared to placebo. Another randomized study revealed that treatment with either nystatin or amphotericin B lozenges resulted in a statistically significant cure rate after 1 month of treatment.
Empiric treatment with topical antifungal drugs (miconazole, clotrimazole, ketoconazole, nystatin) in combination with zinc oxide barrier paste and low-to-mid potency topical corticosteroids (hydrocortisone, fluocinonide, triamcinolone) as needed to control inflammation.
Clotrimazole and miconazole topical preparations may have advantage compared to other antifungal drugs as they have both anti-candida and anti-staphylococcus activity. If patient also has thrush, the oral cavity should be concurrently treated with nystatin solution or systemic fluconazole.
If angular cheilitis is present with honey-colored crusts or the patient has also active atopic dermatitis, bacterial culture should be taken and empiric treatment with antibiotic ointment including: clindamycin, erythromycin or mupirocin should be given.
Topical or intralesional corticosteroid injections may be used as a monotherapy, but if an yeast or bacterial overgrowth is present, such therapy may not be effective.
Surgical treatment for angular cheilitis
Surgical treatment may include:
- Injection of fillers to restore anatomy or repair sulcus at oral commissure. If oral commissures are present with depressions it may be the cause of angular cheilitis promoting, thus injection of dermal filler such as hyaluronic acid may be given as a minimally invasive method to achieve improvement of the local anatomy.
- Reconstructive dental or orofacial repair can be performed in order to correct anatomical abnormalities promoting angular cheilitis
Behavioral treatment for angular cheilitis
Behavioral therapy means behavioral change and cessation of limit lip licking, thumb sucking, flossing, etc. Emollient or barrier zinc-oxide paste should be also given.
Other measures such as: oral hygiene, quiting smoking or other tobacco habits and use of a barrier cream such as zinc oxide paste at night are also recommendable for reversing the local factors and prevention.
Topical corticosteroids for angular cheilitis
Following topical corticosteroids can be used for the treatment of angular cheilitis:
- Hydrocortisone (Cortate, Unicort) 0.5%, 1%, 2.5%
- Amcinonide 0.1%
- Betamethasone valerate (Betnovate, Celestoderm) 0.05%, 0.1%
- Clobetasone butyrate (Eumovate) 0.05%
- Desoximetasone 0.05%, 0.025%
- Flucinonide (Lidex, Lidemol) 0.01%, 0.05%
- Diflucortolone valerate 0.1%
- Fluocinolone acetonide (Synalar, Synamol, Derma-Smooth) 0.01%, 0.025%
- Mometasone furoate 0.1%
- Prednicarbate 0.1%
- Triamcinolone acetonide (Aristocort D, Aristocort, Vioderm-KC, Kenacomb) 0.025% 0.05% and 0.1%
Do antibiotics work well for angular cheilitis?
Topical antibiotics such as clindamycin, erythromycin, mupirocin work for angular cheilitis only if it is caused by Staphylococci or beta-hemolytic bacteria. If the infection is caused due to fungal infection or because of some nutritional deficiency, antibiotics can’t help.
Since most angular cheilitis infections are fungal or fungal/bacterial combination, antibiotics won’t probably done the work alone, thus they are most commonly used in combination with other medicines.
Can OTC clotrimazole cream cure my angular cheilitis?
Clotrimazole cream is OTC medication which is used to treat yeast i and other fungal based infections. Since angular cheilitis can commonly be caused by Candida albicans infections, Clotrimazole antifungal cream can be used for angular cheilitis. However, in some cases in which angular cheilitis are caused by fungal infection or simultaneously by bacterial and fungal infection, clotrimazole OTC product may be ineffective.
So, Clotrimazole might not always be an effective treatment for angular cheilitis. Since you don’t know whether your infection is caused by bacterial or fungal infection or both, it is always the best option to visit your doctor first, before you make your own decisions. In the case of bacterial/fungal coinfection doctor may prescribe the combination of clotrimazole with some topical antibiotic and some barrier paste such as zinc-oxide.
Miconazole for angular cheilitis
Micatin is a Brand name for antifungal medicine containing miconazole as an active ingredient. For angular cheilitis, oral gel formulation of Micatin is very effective. It should be applied twice daily and used two additional days if/when the condition disappears. Miconazole interferes with the synthesis of fungal cell membranes and may also exhibit antibacterial and anti-parasitic properties.
Lamisil for angular cheilitis
Lamisil is a Brand name for antifungal medicine containing terbinafine as an active ingredient. Lamisil shown to be effective medication for angular cheilitis, as it is able to relieve itching, burning, or cracking. It should be applied twice per day, for two weeks or as directed by your doctor. Ensure that any spot of the wound is thoroughly clean before application.
Tinactin for angular cheilitis
Tinactin contains antifungal drug named tolnaftate. It is generally known as a cream that is used against athlete’s foot. But it also shows some efficacy against angular cheilitis. Thus it can be used to eradicate the candida infection around the lips. The area may sting right after beginning of application but should soon go away. It should be administrated twice time a day with monitoring to assume whether the condition is improving.
Zinc Oxide paste for angular chelitis
Zinc oxide paste can be very helpful for repairing the damage of the cracked corners of the mouth. It works especially well if the damage is a result of dehydration. Most doctors prescribe it in combination with topical antifungals, antibiotic and corticosteroid drugs.
If you decide to use zinc oxide cream or ointment, look for a product that has a high % of zinc, at least 20%. Apply it carefully to the cracked corners of your mouth after washing the area. Be careful not to ingest.
Angular cheilitis in children
Angular cheilitis due to bad habits is common in children. Also, children are usually more vulnerable to bad weather conditions and contact dermatitis. However, children are known to have a faster recovery time and rebound faster than others. It is the most common in children who drool while eating or sleeping, those who are sick with weak immunity, or are under a lot of stress.
Angular cheilitis during pregnancy
Since pregnancy causes enormous hormonal and body changes, in a woman body, angular cheilitis can occur at any time during pregnancy, however it is the most common during morning sickness.
Anglular cheilitis in elderly
It seems that this condition is the most common in elderly patients. This might be because elderly generally have weaker immune systems and have excess salivation mostly because of dentures, loss of teeth or other. They also commonly suffer from vitamin deficiencies than younger adults and children.
Can angular cheilitis cause scars?
Semi-permanent scars in the corners of the mouth are possible but rare cause of angular cheilitis. Commonly the scars are not visible until mouth is open. Scars usually look like darker patches of skin in the corners of the mouth. Getting scars is not common, as it is known that human mouth recovers very quickly, unless in the situations when severe angular cheilitis was present or if patient suffer from it frequently.
What should I avoid if I have angular cheilitis?
Patients who have angular cheilitis need to avoid following:
- Touching your mouth. Similar to the acnes or patches, angular cheilitis spots should not be touching. It’s a known habit for many people to touch their face/mouths when thinking, resting their head, etc. You need to keep yourself from touching your mouth in the case of angular cheilitis. The only reason to avoid this is because our hands and fingers are usually dirty and thus wounds should not be touching as it will spread or make the infection worse. Every time you touch your mouth you are potentially introducing new bacteria to the angular cheilitis spot, making it more difficult for your body to heal itself. At least wash your hands before you do so and if you can’t control yourself
- Do not pick the wound. Angular cheilitis wounds are usually gross and unnatractive, especially when they begin to heal. Since, your hands are always the source of new bacteria, especially if they are dirty, you should never pick and touch the wound with them. The best way to get rid of the crust and flaky skin is to wash your hands, then take a warm washcloth, and gently rub it away. Always use different wash cloth if you have angular cheilitis in both corners of your mouth in order to prevent spreading the bacteria across your mouth.
- Never use bleach or other home chemistry products on the wound. Such products usually contain corrosive substances that may irritate your skin, eyes, and respiratory system. Hospital usually uses wound cleaners with a medicinal partial-bleach base to clean serious wounds. Never use your home cleaning products for medicinal purposes.
- Avoid licking and lips nibble, thumb sucking, chewing gums, lollipops. All these actions may increase the salivation and moisture and infection spreading in your mouth, preventing your angular cheilitis to be faster healed.
- Do not use chapstick from a tube. Many patients with angular cheilitis also have chapped lips, so they usually use chapstick frequently for relief. It has to be known that chapstick can make your angular cheilitis worse if used improperly. So, do not use chapstick from a tube because it makes hard pressure. Instead, use soft lip-balm. Chapstick in tube requires more pressure to spread it across your lips. Additionally it may be able to spread the angular cheilitis bacteria and fungus across your entire mouth. If you’re using chapstick from the tube and have angular cheilitis, the best option is to thoroughly clean it or throw it away after use. Thus it is better to use soft lip balm however you may need to apply the balm on your lips with clean fingers. Always take enough of the balm on your finger to avoid re-applying or if you need to do this, use a different finger or wash your hands before the action. Balm should be applied starting from the middle of your lip and then towards to the corners of the mouth. The best way is to end on your mouth corner, because you will prevent spreading and contamination of the bacteria and fungus form your angular cheilitis across your mouth.
- Avoid cold sore medications such as Abreva or Campho-phenique. These products can do nothing for angular cheilitis. They are used for cold sores as they contain drying agent which may dry the skin too much and make your angular cheilitis even worse. Many will tell you that Abreva works perfect for angular cheilitis, however such patients actually have cold sores instead of angular cheilitis, as these 2 conditions are often mistaken.
- Don’t use humidifier for angular cheilitis. Angular cheilitis does not need any extra moisture since it is constantly in contact with the saliva from our mouth.
- Don’t use Neosporin for angular cheilitis. Neosporin is an antibiotic ointment which is used to treat minor cuts, scrapes, and burns on the skin and should not get in touch with your mouth. The only positive indications for Neosporin in angular cheilitis are prevention of scarring on the skin, outside of your mouth in cases where the lesions become severe and split. However there are safer preparations that will do the same or even have far better effects.
- Don’t use topical corticosteroid for a long-term (more than a week) if your angular cheilitis is caused by virus, bacteria or fungal infection. This is something you’re your doctor or pharmacist need to tell you. Topical corticosteroids can be very helpful for the treatment of angular cheilitis and may effectively reduce inflammation symptoms such as swelling, redness, warmth and itching. However, they are imunosupressive agents, and they may make your immune system even weaker if they are used for a long term thus they will make your infection far worse. Never put topical corticosteroid on the open wound, when there is a cut or blood, since corticosteroid may be absorbed into the circulation and may increase the risk of causing side effects. However, it also depends which corticosteroid you use. Low potency topical corticosteroid such as hydrocortisone 0,5% is the safest one. Always use topical corticosteroids according to you doctor recommendation.
Can Vitamin B complex supplements heal my angular cheilitis?
In some cases angular cheilitis can be caused or provoked by some of vitamin B deficiency (especially vitamin B2). Having adequate amount of vitamin B, especially riboflavin (vitamin B2) in your body will probabbly help you to heal your angular cheilitis faster than if you didn’t take any vitamin B supplements. However, vitamin B complex monotherapy won’t heal this condition alone.
Is Carmex effective for angular cheilitis?
Carmex lip balm has been shown to be effective for healing chapped lips and is also commonly used to treat cold sores. However, the cause of angular cheilitis is more complex than in the case of cold cold sores and chapped lips, therefore Carmex won’t be able to heal angular cheilitis, but it may be helpful for temporary relief.
Be cautious when applying Carmex since angular cheilitis is mostly fungal/bacterial based, so, when you apply the Carmex across your lips you can accidentally spread the bacteria/fungus across your entire mouth especially in the case if you have angular cheilitis only on one side of your mouth, it will easily spread to the other corner of by doing this.
Is Candex effective for angular cheilitis?
Candex is a Brand name for enzymes that can fight fungal infections. It may help to prevent angular cheilitis, but is generally used for more severe forms of yeast infection. Candex is however not recommended as a first line treatment for angular cheilitis because only about 20-25% of angular cheilitis is caused by fungus.
Is Blistex helpful for angular cheilitis?
Blistex is a Brand name for a lip balm that contains dimethicone or polydimethylsiloxane/PDMS as an active ingredient. Dimethicone is a silicone-based polymer. It is form of silicone oil that has a very smooth application.
Dimethicone does not have antibacterial nor antifungal properties thus it won’t be able to eradicate the infection responsible for your angular cheilitis. But it may be helpful as it helps to prevent transepidermal water loss, enabling the patients to retain moisture in a proper way.
This product also contains oxybenzone and padimate as active ingredients. Oxybenzone is a benzophenone compound that protects against UVB rays and some UVA rays. Padimate is a derivative of paraminobenzoic acid, and provides sun protection as well. As lips can burn in the sun, Blistex may offer a good defence to the sensitive area of lips.
So, Blistex alone can’t eradicate infection, but it can be effective when used in combination with other medicines.
What natural moisturizers can I use for my angular cheilitis?
Glycerin, Vaseline, Cocoa butter, Coconut oil and Olive oil are natural moistruizers that can be helpful for your angular cheilitis
Glycerin should be applied to affected areas 3-4 times a day. It is able to relieve the pain associated with angular cheilitis and also promote the healing process.
Vaseline is able to prevent air contact when covering the affected areas. Apply as needed basis, especially if you are going out during cold and windy weather. Vaseline can easy your pain and keep the area of angular cheilitis protected from further chapping.
Cocoa butter is a good moisturizes so applying it 2-3 times per day should help dealing with cracked lips, fighting the infection and moisturizes to prevent additional events of this issue.
Coconut oil has been shown as an excellent natural remedy for treating angular cheilitis. It acts as a good moisturizer and removes dryness of the lips. It also contains antibacterial and antifungal properties. Apply coconut oil 2-3 times a day for best results.
Due to its antibacterial properties, olive oil has been used for threating different skin conditions for centuries. Because of its excellent moisturizing properties it can be used for the treatment of angular cheilitis. Warmed olive oil should be mixed with a few drops of lemon juice, and then applied to the affected areas 3-4 times per day.
Can sun, saltwater and chlorine cure my angular cheilitis?
Many patients have been reported that their angular cheilitis was becoming significantly better or in some cases even completely healing during vacationing on the sea. Since sea water is known to its healthy skin properties for thousands of year this should not be surprise.
The high mineral content of sea water containing sodium, chlorine but also other minerals may be absorbed by the skin and may soothe health problems including eczema, bug bites, poison ivy, etc.
It does not mean that sea water can also cure angular cheilitis alone, but actually the combination salt water, chlorine and sun may help with angular cheilitis, especially if it is known that most bacteria can’t survive in salt water as salt causes dehydration of bacteria’s cell membranes and its rupture. The salt will certainly also help to dry the wounds of angular cheilitis.
Also the combination of salty water and especially the sun have fantastic antifungal outcomes. Yeast needs a dark, moist and warm environment to survive, and those who are swimming in seas and pools will receive a lot of sunlight. Thus sun exposure will have a negative effect on any yeast including those on angular cheilitis wounds.
What natural remedies can I use for my angular cheilitis?
Water and angular cheilitis
It is important to get hydrated enough during the day. Dehydratation is known as a predisposed factor of angular cheilitis. It is recommended to drink 10 to 12 glasses of water per day to minimize risk of dehydration and keep the systems working.
Baker soda and angular cheilitis
Paste made by baking soda and water can be very helpful for treating angular cheilitis when applied to the affected area. After applying it should stay to dry for some minutes. You can apply some moisturizer after washing it, to avoid dryness of the region.
Lemon and angular cheilitis
It is known that lemon contains antioxidant properites. Although it may cause some irritation and tingling when applied to the affected area it should effectively fight bacteria.
Cucumber and angular cheilitis
The coolness of the cucumber can be helpful for pain relieving. Slices of washed and cold cucumber can be applied on the affected area of the skin.
Tea tree oil and angular cheilitis
This oil is known for its antibacterial, antiviral and antifungal properties. The best way to use it is to take 1 tablespoon of it mixed with 1 teaspoon of vitamin E oil and applied 4-5 times a day to promote the healing of the wound faster.
Aloe Vera and angular cheilitis
You can use any form of aloe vera plant (extract, solution, leafs etc) if you are not allergic to it. Refrigerate a leaf of Aloe Vera for one hour and then gently rub across the affected area 3 times a day for best results. Aloe Vera should relieve the pain and also help promote healing. However, in some people contact dermatitis may be developed, thus all Aloe vera preparations should be used with caution for the first time.
Honey and angular cheilitis
Honey is well known due to its antibacterial properties. Honey may resolve the low-mid overbalance of the bacteria or fungus causing the angular cheilitis. Apply the honey on the affected area and leave for 15 minutes.
Margosa leaves and angular cheilitis
These leaves have been show as an effective treatment for cracked corners caused by angular cheilitis. The powder of Margosa leeaves can also be applied directly to the affected areas.
Yoghurt and angular cheilitis
Probiotics properties, protein source and cooling effects of the refrigerated yoghurt can be helpful for angular cheilitis symptoms. You can apply it during the night and let it to do the job.
Listerine and angular cheilitis
Because of excellent antifungal and antibacterial properties Listerine may be helpful. Wash the wound 2-3 times with Listerine during the day.
Active oxygen and angular cheilitis
Treatment with active oxygen provide excellent results, as it is able to effectively fight bacteria, viruses and fungi that will be eliminated along with dead skin cells and stimulates the regeneration of existing healthy cells. For best results, apply at at least 2 and up to 4 times a day on affected areas.
What diet changes should I make for angular cheilitis?
The diet always plays important in any health condition you have. Patients with angular cheilitis should avoid spicy, warm, heavy and sour foods that can irritate the cracks of their mouth. Sugar and caffeine may also be problematical. These types of foods may dehydrate the body slow down the healing. The general diet recommendations for angular cheilitis are:
- Take enough water and other fluids (10 glasses a day) in order to stay hydrated during the day.
- Follow a healthy and balanced diet comprising of a variety of different foods.
- Consume lots of fresh fruits and vegetables as these are rich in antioxidants
- Have vitamins and minerals rich foods in order to stay healthy and faster heal Angular cheilitis.
- Vitamin and minerals supplements can also be taken. Especially vitamin B complex, vitamin C (500-1000 mg), Zinc, Iron, vitamin E.
- Vitamin C is very important as it helps to guard the body from sun damage and also aids in tissue refurbishing.
- Leafy vegetables, nuts and eggs contain high amounts of vitamin E which is powerful antioxidant and helps to drying of the skin.
“What causes blood in the stool? Hematochezia (rectal bleeding) treatment“