Contents
- What is dermatofibroma?
- Different names for dermatofibroma
- Dermatofibroma signs and symptoms
- Dermatofibroma incidence
- Different types of dermatofibroma
- What causes dermatofibroma?
- Dermatofibroma diagnosis
- Dermoscopy for dermatofibromas
- Differential diagnosis for dermatofibroma
- What is dermatofibroma prognosis?
- Dermatofibroma treatment
- Dermatofibroma surgical care
- Dermatofibroma freezing treatment
What is dermatofibroma?
Dermatofibroma or superficial benign fibrous histiocytoma are common and benign skin tumours which are more precisely describe as cutaneous soft-tissue lesions. The prevalence of dermatofibroma is about 3% of skin lesion examples received by dermatopathology laboratories. It is more frequent in adults and occurs more commonly in women.
It is most commonly located on the extremities usually at lower legs and is typically asymptomatic, although pruritus and tenderness can be present. The true cause of dermatofibroma is not known, but it is broadly accepted that it may result from a trauma including insect bite, follicular cyst and follicle rupture. There are some evidences supporting the neoplastic nature of the tumor.
A several histologic subtypes of dermatofibroma have been desribed. Tumor usually do not need removal unless diagnostic is uncertain and if particularly troubling symptoms are present.
Different names for dermatofibroma
In medical literature there are different names for dermatofibroma, such as:
- Benign fibrous histiocytomas
- Dermal dendrocytoma
- Fibrous dermatofibroma
- Fibrous histiocytoma
- Fibroma simplex
- Nodular subepidermal fibrosis
- Sclerosing hemangioma
Dermatofibroma signs and symptoms
Dermatofibroma characteristically looks like a fixed, slowly growing most commonly lonely red, pink or purple to brown nodules, papules or plaques that are usually located on the lower extremities but may also appear on trunk and arms. The surface can be smooth and shiny, or keratotic. The size of lesions may range from a few millimeters to >2 cm.
However, there are several clinical variants of multiple and giant dermatofibroma such as hemosiderotic dermatofibroma. In some, not so common cases pruritus and ulceration may represent related symptoms.
On palpation, a typical dimple-like depression in the overlying skin can be produced after pinching the lesion gently. Dermatofibroma is known to be persistent lesion; however it may shrink during the time and regress as a hyperpigmented, and to looks-like a macule.
As a conclusion, typical manifestations of dermatofibroma are raised, small and hard skin growths that are:
- Most commonly localize on lower legs, but may also appear on the arms or trunk
- Color may be red, pink, purple-like, gray or brown and may be changed over time
- Usually small in size and rarely grow larger than a fingernail
- Painless but may be tender, painful or itchy
- Usually dimple inward when pinched
Dermatofibroma incidence
Dermatofibromas are relatively common skin condition. Frequency of dermatofibroma seems to be similar in all races. Females are more commonly affected by dermatofibroma than males, with a male-to-female ratio of 1:2, or even higher. It can occur in patients of all ages, however in 80% it most commonly affect patients of ages between 20-49 years. They are more common in immune-compromised patients.
Different types of dermatofibroma
There are several different types of dermatofibroma which are basically distinguished by their histopathological findings. Though, it is important to know that there were cases of dermatofibroma where the histological features of several variants coexisting in the same lesion were desribed. Some of these variants also have different clinical findings as well as different rates of local recurrence, thus making correct diagnosis very important.
Rare cases of metastasis have also been reported. More studies are needed to confirm the variants of metastatic dermatofibromas and for now they are considered as benign tumors.
Except common dermatofibroma which is described above, there are also other variants of such as:
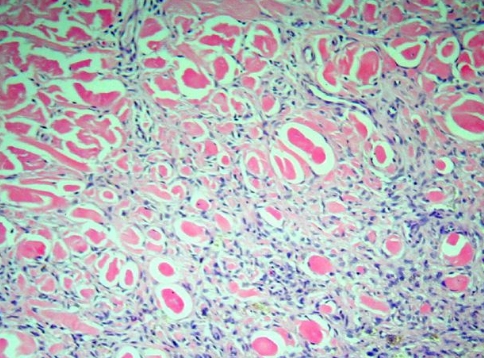
- Aneurysmal dermatofibroma. This variant usually appears in less than 2% of dermatofibromas. Its clinical presentation can be a bit different compared to common dermatofibroma and most frequently looks like blue-brown nodule on the limbs. If bleeding of such nodule occurs it may start to grow rapidly thus clinical misdiagnosis with a vascular or melanocytic lesion is common.After removal, their rate of recurrence is about 19%. Histologically, the most characteristic feature is the presence of irregular hemorrhagic spaces without endothelial lining.
- Hemosiderotic dermatofibroma. This type is described in about 5% of cases with dermatofibroma. It probably represents a stage in the aneurysmal dermatofiborma development. The lesion is composed of several small vessels, erythrocytes and intra- and extracellular hemosiderin deposition caused by bleeding. Acanthosis was also observed in patients with hemosiderotic dermatofibroma. Differential diagnosis should be always done in order to exclude melanoma as well as other melanocytic and nonmelanocytic lesions.
- Epithelioid dermatofibroma. This variant is more common in man. Clinically, it is represented as a polyp red nodule, located mostly on the limbs, thus it may be misdiagnosed with pyogenic granuloma. Histologically, it is described as a demarcated lesion in the superficial and papillary reticular dermis surrounded by an epidermal collarette. The occurrence of numerous small vessels placed among epithelioid cells is also a common feature. The most important differential diagnosis should be done with Spitz nevus. Differently from Spitz nevus, epithelioid dermatofibroma has no junctional component or nesting and the cells are almost always negative for melanocytic markers.
- Cellular dermatofibroma. This type of dermatofibroma usually appears in less than 5% of cases.Similar to epithelioid variant, cellular dermatofibroma is also slightly more common in male population. Despite its prevalence on extremities, it may also develop on unusual sites, including face, ears, feet and hands. Recurrence rates can be developed in 25% of cases. Metastasis to regional lymph nodes and lungs has been also reported in some not so common cases. Histologically, the lesions are extremely cellular with a more noticeable fascicular development. Lesional cells aim to have more profuse eosinophilic cytoplasm and generally are very infiltrative. Differential diagnosis should be made for dermatofibrosarcomaprotuberans and leiomyosarcoma.
- Lipidized dermatofibroma. This type of dermatofibroma is very rare. It is also known as “ankle-type” dermatofibroma because of its appearing on the legs especially around the ankles. Clinically, it is representing as a solitary yellow nodule usually larger compared to common variant.Studies have been showed no relations with hyperlipidemia. Histologically, it is described with a presence of foamy macrophages surrounded by abundant sclerotic collagen bundle. The prognosis of this variant appears to be very good, with no recurrence even after excision is incomplete.
- Atrophic dermatofibroma. Although very rare, it probably characterizes the end-stage of common dermatofibroma. Clinically, it is present as an area of retraction, often resembling a scar, anetoderma or basal cell carcinoma. Atrophic dermatofibroma is easily recognized by its dermal atrophy with prominent sclerotic collagen and low cellularity.
- Clear cell dermatofibroma. This variant is considered as the rarest. The dermatofibroma lesion usually contains sheets of clear cells with vesicular nuclei that inhabit the reticular dermis and may extend into the subcutis. Differently from all other dermatofibroma types, clear cell fibrous dermatofibroma is not related with epidermal changes. It has to be differentiated from renal cell carcinoma metastasis and clear cell sarcoma.
What causes dermatofibroma?
The true cause of dermatofibroma is still unknown. However, it is usually attributed to be a responsive process to some skin traumas such as arthropod bite, states after folliculitis, tattooing, tuberculin skin testing. Clonal analysis also suggests that dermatofibroma may represent a true neoplasm.
Common dermatofibromas contain a combination of fibroblasts, macrophages and blood vessels. Most cases involve only the dermis but it may also extend to the subcutis. Altered immunity possible has an important role in many cases of multiple eruptive dermatofibromas related with different underlying conditions and medications.
Some studies have been also found that genetic component may exist.
Dermatofibroma diagnosis
- Diagnosis is usually confirmed after physical examination and palpitation of the lesion, as few other skin lesions are as firm.
- The pinch test may be also very helpful but not definitive for diagnosis confirmation as squeezing the lesion from the sides results in dimpling of overlying skin.
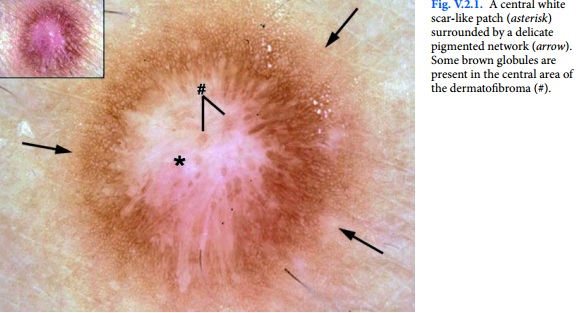
- With a dermatoscope, dermatofibromas characteristically express a pigment network and central white patch but there is considerable difference. One study noted a difference in dermatoscopy look depending on location of the lesion.
- Excision biopsy is always useful where diagnostic doubt remains after examination
- A study of localized skin lesions imaged through the variable-frequency ultrasound included the image of a hypoechoic solid nodule created by a dermatofibroma. Dermatofibromas have been analyzed by high-definition optical coherent tomography.
- Dermatofibroma can mimic a malignant lesion on fluorodeoxyglucose positron-emission tomography (FDG-PET) scans.
Dermoscopy for dermatofibromas
Dermoscopy may be very useful adjunctive diagnostic technique for dermatofibromas. The most common pattern seen is a peripheral pigment network with a central white area.
Dermoscopy of a xanthomatous dermatofibroma demonstrates a homogeneous pattern with yellow shades and a peripheral pigment network. A green color may be a good indicator of the hemosiderotic dermatofibroma. If a indicative melanocytic or atypical pattern is noted with dermoscopy, a diagnostic biopsy should be performed.
Differential diagnosis for dermatofibroma
Differential diagnosis should be made for following similar skin conditions:
- Acrochordon
- Anal polyp
- Angiomatoid fibrous histiocytoma
- Atypical Fibroxanthoma
- Atypical Mole (Clark Nevus or Dysplastic Nevus)
- Basal Cell Carcinoma
- Blue Nevi
- Cutaneous Manifestations of HIV
- Cutaneous Melanoma
- Cutaneous Squamous Cell Carcinoma
- Cutaneous T-Cell Lymphoma
- Cylindroma
- Dermatofibrosarcoma Protuberans
- Dermatologic Manifestations of Juvenile Xanthogranuloma
- Cutaneous Lipomas
- Dermatologic Manifestations of Merkel Cell Carcinoma
- Dermatologic Manifestations of Metastatic Carcinomas
- Dermatologic Manifestations of Neurilemmoma (Schwannoma)
- Epithelioid sarcoma
- Erythema Elevatum Diutinum
- Infantile Digital Fibromatosis
- Keloid and Hypertrophic Scar
- Keratoacanthoma
- Leiomyoma
- Mastocytosis
- Melanocytic Nevi
- Multicentric Reticulohistiocytosis
- Multinucleate Cell Angiohistiocytoma
- Pilomatrixoma
- Plaquelike myofibroblastic tumor
- Prurigo Nodularis
- Spiradenoma
- Spitz Nevus
- Supernumerary Nipple
- Targetoid Hemosiderotic Hemangioma
What is dermatofibroma prognosis?
Typical dermatofibromas are considered non-malign lesions, and the prognosis for patients with common dermatofibromas is excellent. However, discomfort from pain or itching may be caused.
However, deep, cellular, aneurysmal, hemosiderotic and atypical types of dermatofibroma can be recurrent in almost every 5th patients, and they can also rarely metastasize. Such variants, or any indeterminant dermatofibroma, might be considered as potentially malignant tumors.
Although rare, in these particular cases pulmonary and nodal metastases were most commonly seen and some patients developed multiple satellite nodules, and deaths have occurred.
The primary tumors aimed to be cellular type, they are usually large, and however aggressive behavior is not predictable, although early or frequent reappearances of the tumor after incision should raise concern. Array-based comparative genomic hybridization (CGH) may prove useful in identifying these higher-risk variants.
The epithelioid type of dermatofibroma has also been reported to be able to metastasize.
Spontaneous regression has been reported and this may yield postinflammatory hypopigmentation, although this appears to be very rare.
Dermatofibroma treatment
There are no medications for dermatofibroma treatment, not any are recommended. Also in most cases no treatment is necessary. Simple diagnostic reassurance that the skin tumor/lession is benign may be indicated, unless some of the aggressive subtypes are doubted or diagnosed. In those with dark skin, liquid nitrogen freezing or steroid injection of may cause pigmentary change but they are usually temporary.
Intralesional steroid injections have been attempted with no-adequate results. Surgical treatment is the only way to get rid of dermatofibroma and it is most commonly very effective option
Dermatofibroma surgical care
For patients who have cosmetically unacceptable lesions, in those whose dermatofibroma is symptomatic with intese tenderness and pruritus, or in cases where there is diagnostic doubt, or when aggressive variants are suspected, complete surgical excision, including the subcutaneous fat, is recommendable and ideal procedure. Obtaining a 3mm sideline has been shown to completely remove common type dermatofibromas.
It has been shown that one aggressive type of dermatofibroma called aneurysmal dermatofibroma, can be successfully treated with Mohs micrographic surgery.
An inverted pyramidal biopsy technique may allow for an aesthetically pleasing result, while still providing acceptable tissue for histologic findings.
Cryosurgery or superficially shaving can be attempted; however, recurrences are more likely.
Carbon dioxide and pulsed-dye laser treatments have been also used successfully in the dermatofibroma management.
If during surgical removal, the dermatofibroma is not removed completely and significant change occurs in the size, color, borders or symptoms, the patient should seek follow-up evaluation. If complete removal has been done, patients with lesions that recur also should seek follow-up evaluation.
An aggressive subtype or another diferentiate diagnosis should be ruled out. If multiple lesions develop with eruptive symptomatology, screening for a family history of this and for underlying related diseases and drugs should be considered.
Dermatofibroma freezing treatment
Some health care professionals use liquid nitrogen freezing methods to treat and remove dermatofibroma. During this procedure, liquid nitrogen is used to freeze dermatofibroma and flatten it to the level of the skin. Though, this method usually leaves behind a white scar. There are also chances of reoccurrence after treatment.
“What does a lupus rash look like? Is lupus life threatening disease?“