Contents
- What is naloxone?
- What is molecular formula, weight, structure and category of naloxone?
- What is IUPAC name of naloxone?
- How effective is naloxone?
- Why is naloxone prescribed?
- What are approved indications for naloxone use?
- How does naloxone work?
- What are brand names of naloxone?
- Naloxone absorption
- How naloxone is distributed in the body?
- Metabolism and elimination of naloxone
- What are the contraindications of naloxone?
- What should I discuss with my health care provider before using naloxone?
- How should naloxone be used?
- Naloxone dosage for different indications
- What happens if I miss a dose of naloxone?
- What happens if I overdose naloxone?
- What should I avoid while using naloxone?
- What are the side effects of naloxone?
- Does naloxone only work for overdose cases caused by opioids?
- Is naloxone dangerous?
- Will naloxone make you high?
- Can you overdose on buprenorphine? Will naloxone stop such an overdose?
- Will naloxone work even if someone has previously used it?
- Is naloxone the same as naltrexone?
- Can naloxone be safely used if it is expired?
- Are there other ways to use naloxone besides injecting it?
- Can naloxone cause seizures?
- What is the most important information I should know about naloxone (Narcan)?
- Can patients with cardiovascular disorders take naloxone?
- Can patients with liver disease take Naloxone?
- Can patients with renal disease take Naloxone?
- Can patients with septic shock take Naloxone?
- Should a patient with high blood pressure take Naloxone?
- What are withdrawal effects that are associated with Naloxone use?
- Can I take Paracetamol after naloxone?
- What common medications interact with Naloxone?
- What are the cautions needed for administration of Naloxone?
- Use of naloxone in pregnancy & lactation
- Naloxone and droperidol
- Naloxone and fentanyl
- Naloxone and codeine
- Naloxone and Oxycodone
- Naloxone and morphine
- Can diazepam be given with naloxone?
What is naloxone?
Naloxone is a generic name of an opioid antagonist medication used to block or reverse the effects of opioid drugs, particularly within the setting of drug overdoses which are rapidly becoming a leading cause of death worldwide. Naloxone blocks or reverses the effects of opioid medication, including extreme drowsiness, slowed breathing, or loss of consciousness.
It is also used for diagnosing whether a person has used an overdose of an opioid. It’s also one of the active ingredients in combination prescription drugs that contain two or more active ingredients, like Bunavail, Suboxone, and Zubsolv.
Naloxone works by preventing drugs or substances in the opium family from binding to areas outside of cells where they normally have an effect. The Food and Drug Administration (FDA) first approved naloxone under the brand name Narcan in 1971, originally manufactured by Endo Pharms. The Narcan brand was later discontinued in the United States.
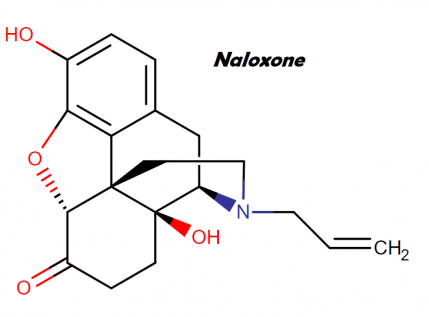
What is molecular formula, weight, structure and category of naloxone?
Molecular Formula: C19H21NO4
Molecular weight: 327.38 g/mol
Naloxone structure:
This compound belongs to the class of organic compounds known as phenanthrenes and derivatives. These are polycyclic compounds containing a phenanthrene moiety, which is a tricyclic aromatic compound with three non-linearly fused benzene.
What is IUPAC name of naloxone?
Naloxone IUPAC name is: (4R,4aS,7aR,12bS)-4a,9-dihydroxy-3-prop-2-enyl-2,4,5,6,7a,13-hexahydro-1H-4,12-methanobenzofuro[3,2-e]isoquinoline-7-one
How effective is naloxone?
Naloxone is a medication that starts working within minutes and is very effective. Its efficacy depends upon the dosage of drug taken. It may several doses in case of powerful opioids such as fentanyl. Naloxone is not addictive and fewer side effects.
Naloxone does not effect on any other type of overdose and works only if the opioid is already in the system of a person. It cannot even prevent an overdose of any medicine.
Within 20 to 90 minutes, the effects of naloxone can wear off completely. So, it should be used immediately in case of narcotic overdose.
Why is naloxone prescribed?
Naloxone is prescribed for:
Opiate overdose and associated depression
- Some natural and synthetic opiates named anileridine, codeine, diphenoxylate, fentanyl, heroin, hydromorphone, levorphanol, meperidine, methadone, morphine, oxymorphone, concentrated opium alkaloids hydrochlorides, and propoxyphene, cause depression including respiratory depression can be treated with the help of naloxone.
- It is also useful for the treatment of opiate-induced respiratory depression, caused by certain opiate partial agonists such as butorphanol, nalbuphine, pentazocine, and cyclazocine. However, higher and frequent doses of naloxone may be required for reversal of respiratory depression resulting from over dosage of opiate partial agonists.
- Naloxone is also useful for emergency treatment of suspected opiate overdose which may be identified with the help of respiratory or CNS depression. Family members of a patient who had overdose of opiate can also provide immediate treatment as naloxone is available as auto-injector and nasal spray.
- Efforts should be done in order to provide easy access of naloxone to community based programs for substance users. It should be made available to family members of the patients who are at increased risk of opiate overdose or who are receiving opiate analgesic, those receiving benzodiazepines or other sedatives, It should be made available to the places where overdoses of opioids may be witness for example: nursing homes, home visiting nurses, outreach patients, and substance abuse treatments etc.
- Naloxone is also useful for the treatment of mild to moderate as well as severe opiate-induced depression mainly respiratory depression.
- One should make sure that the administration of naloxone should be accompanied along with other resuscitative measures (administration of oxygen, mechanical ventilation, or artificial respiration).
- Other more immediate supportive treatment should be initiated because duration of respiratory depression after opiate agonist over dosage may be longer than the duration of naloxone.
- The withdrawal symptoms cannot be readily suppressed even after the persistence of naloxone action, in patients who are physically dependent on opiate agonists.
- The patient taking the naloxone may show severe symptom after few minutes to 30 minutes of administration and the effects are precipitated in patient showing opiate abstinence syndrome.
- Some value in the management of buprenorphine over dosage but should notbe relied on for treatment of respiratory depression. Reversal of agonist effects develops slowly.
Diagnosis of opiate overdosage
In the absence of confirmed history or clear diagnostic clinical findings, naloxone aids in diagnosis of suspected acute opiate over dosage.
Diagnosis of chronic opiate abuse
This is also called as naloxone challenge test, and used as an aid in the diagnosis of chronic opiate abuse. Naloxone can precipitate the withdrawal symptoms in patients who are physicaly dependent on opiates; therefore it is preferred to use chemical methods to detect the presence of opiates in urine.
In patients who have completed detoxification, before induction of naltrexone therapy the naloxone challenge test (also called screening test) should be done. Such screening can avoid precipitating opiate withdrawal after administration of naltrexone.
Clonidine induced coma
Naloxone is also used to reverse Clonidine-induced coma and respiratory depression.
Detoxification and maintenance treatment of opiate dependence
- For detoxification or treatment of opiate dependence the combination of methadone hydrochloride and naloxone hydrochloride in a ratio of 20:1 has been administered orally. It should be used along with other appropriate medical services.
- It reduces the desire of opiates by preventing the euphoria created by the administration of opiates.
- Naloxone is also used in management of opiate withdrawal for rapid and ultra rapid detoxification in patients dependent upon opiates. The rapid opiate detoxification involves the administration of opiate antagonists such as naloxone or naltrexone to shorten the duration of detoxification.
- Ultra detoxification is similar but it is done when the patient is sedated or under the effects of anesthesia.
- While considering the naloxone or opiate withdrawal treatment, one should consider complete costs (including the cost of general anesthesia and hospitalization) and adverse respiratory and cardiovascular effects.
Minimize the pentazocine or buprenorphine abuse potential
In order to minimize abuse potential of pentazocine or buprenorphine hydrochloride, naloxone should be used orally in fixed combination with pentazocine hydrochloride or buprenorphine. The antagonistic effect of naloxone will predominate if the combinations are administered parenterally and/or if usual oral doses are exceeded.
Adjunctive use in septic shock
In order to increase the blood pressure in the management of septic shock, the naloxone has been used as adjunctive therapy in few patients. It is not observed as beneficial in improvement of survival however, it shows rise in BP that may lasts up to several hours.
What are approved indications for naloxone use?
FDA approved indications for naloxone are:
- Opioid Dependence
- Opioid Overdose
- Pruritis
- Respiratory Depression
- Severe Pain
- Shock, Septic
- Moderate Pain
How does naloxone work?
Naloxone is a thebaine derivative that holds strong and competitive opioid antagonistic properties. Naloxone binds to the opioids receptor in the CNS thereby reverses the effect of opioid analgesic. It inhibits the actions of opioid analgesic that includes analgesia, euphoria, sedation, respiratory depression, miosis, bradycardia, and physical dependence. Naloxone have high affinity to mu-opioid receptors in CNS whereas lesser affinity to kappa and gamma-opioid receptors in CNS.
Naloxone reverses the effects such as respiratory depression, sedation, and hypotension associated with opioids intake as naloxone is an opioid antagonist. Naloxone can also antagonize the effects of pentaocine which cause psychomimetic and dysphoric effects. Naloxone does not possess agonistic or morphine like properties or characteristics of other narcotic antagonists.
It exhibits essentially no pharmacologic activity, in the absence of narcotics or agonistic effects of other narcotic antagonists. The onset of action is apparent within 2 minutes, when given intravenously. The onset of action is slower if given subcutaneously or intramuscularly. The duration of action also differs between sites of injection and dose.
What are brand names of naloxone?
Naloxone is most commonly available at the market at following Evzio, Narcan Nasal Spray, Narcan Injection.
Naloxone absorption
Naloxone is poorly absorbed when taken by mouth, so it is commonly combined with a number of oral opioid preparations, including buprenorphine and pentazocine, so that when taken orally, just the opioid has an effect, but if misused by injecting, the naloxone blocks the effect of the opioid.
How naloxone is distributed in the body?
Naloxone is rapidly distributed in the body and readily crosses the placenta, following parenteral administration. A relatively weak plasma protein binding occurs. Plasma albumin is the major binding constituent but significant binding of naloxone also occurs to plasma constituents other than albumin. There have been no reports noted if naloxone excreted in milk or not.
Metabolism and elimination of naloxone
As a major metabolite, naloxone is metabolized in liver by glucuronide conjugation with naloxone-3-glucuronide. In adults, a serum half life ranged from 30 to 81 minutes as per one study whereas in a neonatal study, the plasma half life was observed to be 3.1 ± 0.5 hours. 25% to 40% of drug excreted as metabolites in urine after oral or intravenous dose within hours of administration and about 50% in 24 hours and 70% in 72 hours.
What are the contraindications of naloxone?
Naloxone is contraindicated in patients who are hypersensitive to naloxone. Any other ingredient in the formulation should also be checked for hypersensitivity in the patients.
What should I discuss with my health care provider before using naloxone?
You should not use this medication if you are allergic to naloxone.
If possible before you receive naloxone, tell your doctor if you have:
- Heart disease
- Seizures
- History of head injury
- History of drug or alcohol addiction
How should naloxone be used?
Naloxone injection is injected into a muscle or under the skin, or into a vein through an IV. This injection should be administered in a hospital or a health clinic in order to prevent immediate side effects if any. Some vital functions such as breathing, blood pressure, oxygen levels, and kidney function should be watched closely while receiving naloxone. Such identifications also help your doctor to determine that if you can use this medication for longer time period.
Naloxone hydrochloride injection may be administered intravenously, intramuscularly, or subcutaneously. The intravenous administration is effective in achieving most rapid onset of action and is recommended in emergency situations. The patient should be kept under continued surveillance, because the duration of action of some opioids may exceed that of naloxone
Naloxone dosage for different indications
Naloxone hydrochloride injection may be administered intravenously, intramuscularly, or subcutaneously. The intravenous administration is effective in achieving most rapid onset of action and is recommended in emergency situations. The patient should be kept under continued surveillance, because the duration of action of some opioids may exceed that of naloxone. If necessary, the dose of naloxone should be repeated.
Intravenous infusion:
Naloxone hydrochloride injection may be diluted for intravenous infusion. It should be diluted for 0.9% sodium hydrochloride injection or 5% dextrose injection. A concentration if 0.004 mg/ml can be made with 2 mg of naloxone hydrochloride in 500 ml of any of above solution. The mixture should be sued within 24 hours. The remaining solution after completion of 24 hours should be discarded. The rate of administration should be titrated in accordance with the patient’s response.
Naloxone Hydrochloride Injection should not be mixed with preparations containing bisulfite, metabisulfite, long-chain or high molecular weight anions, or any solution having an alkaline pH. Unless the effect of naloxone on chemical and physical stability of the solution has been established, one should not add any drug or chemical to the naloxone hydrochloride injection.
General:
One should not administer this medication, until the solution is clear and container is intact.
In order to check the presence of particulate matter and discoloration, the parenteral drug solution should be checked visually before administration.
Usage in adults:
Opioid Overdose – Known or suspected:
Naloxone hydrochloride should be administered intravenously in an initial dose of 0.4 mg to 2 mg. The dose may be repeated, if the desired improvement in symptoms have not obtained. The dose of naloxone hydrochloride should be repeated at the interval of two to three minutes. Opioid induced or partially opioid induced toxicity should be questioned if no response is observed even after 10 mg of naloxone hydrochloride have been administered. If intravenous route is not available, the intramuscular or subcutaneous route should have considered.
Postoperative opioid depression:
Smaller doses of naloxone hydrochloride are usually sufficient for the partial reversal of opioid depression after use of opioids during surgery. The dose of naloxone hydrochloride should be adjusted as per patient’s response.
- Naloxone hydrochloride should be injected in increments of 0.1 to 0.2 mg intravenously at an interval of 2 to 3 minutes, for an initial reversal of respiratory depression, until the desired level of reversal is achieved.
- Level of reversal can be checked by the adequate ventilation and alertness without significant pain or discomfort.
- Naloxone can never be administered for larger than necessary dose as it can result in significant reversal of analgesia and can cause sudden increase in blood pressure.
- Too rapid reversal can cause vomiting, sweating, or circulatory stress.
- Depending upon the amount, type, and time interval from last administration of opioid, patient may need repeated doses of naloxone within 2 to 4 hour intervals. The longer lasting effect can be produced by supplemental intramuscular doses.
Septic Shock: The optimal dosage of naloxone or duration of therapy for the treatment of hypotension in septic shock patients has not been established
Usage in Pediatric Population:
Opioid Overdose – Known or Suspected:
- The usual initial dose in children is 0.01 mg/kg body weight given intravenously.
- A subsequent dose of 0.1 mg/kg body weight may be administered, if this dose does not result in the desired degree of clinical improvement.
- Naloxone may be administered intramuscularly or subcutaneously in divided doses, if an intravenous route of administration is not available.
- Naloxone hydrochloride injection can be diluted with sterile water for injection, if necessary.
Postoperative Opioid Depression: Follow the recommendations and cautions under
Adult Postoperative Opioid Depression. For the initial reversal of respiratory depression naloxone hydrochloride should be injected in increments of 0.005 mg to 0.01 mg intravenously at two to three minute intervals to the desired degree of reversal.
Usage in Neonates: When using naloxone hydrochloride injection in neonates a product containing 0.02 mg/ml should be used.
Opioid-Induced Depression: The usual initial dose is 0.01 mg/kg body weight administered intravenously, intramuscularly or subcutaneously. This dose may be repeated in accordance with adult administration guidelines for postoperative opioid depression
What happens if I miss a dose of naloxone?
You will always receive a dose of naloxone in emergency therefore there are you are not likely to miss a dose.
What happens if I overdose naloxone?
In such situation, let your doctor know about the situation and always seek for emergency medical help or medical treatment. As overdose can impair person’s thinking and reactions.
What should I avoid while using naloxone?
After giving a naloxone injection, a patient should not be left unattended.
What are the side effects of naloxone?
Get emergency medical help if you have signs of an allergic reaction to naloxone: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Because naloxone reverses opioid effects, this medicine may cause sudden withdrawal symptoms such as:
- nausea, vomiting, diarrhea, stomach pain;
- fever, sweating, body aches, weakness;
- tremors or shivering, fast heart rate, pounding heartbeats, increased blood pressure;
- feeling nervous, restless, or irritable;
- goose bumps, shivering;
- runny nose, yawning; or
- (In babies younger than 4 weeks old) seizures, crying, stiffness, overactive reflexes.
Does naloxone only work for overdose cases caused by opioids?
Yes. Naloxone is used for reversal of effects of opioids such as heroin, methadone, morphine, opium, codeine, or hydrocodone only. There are many other medications whose effects does not counteract by naloxone, such medications include: benzodiazepenes (ncluding diazepam, midazolam, or alprazolam), antihistamines such as phenergan or pheniramine, alcohol or other sedatives, stimulants (such as cocaine and amphetamines).
In case of absence of breathing, naloxone will not hurt. In case of administration of opioids, the patient may regain the breathing, though the sedation remains the same that occurred from other drugs. Many overdoses happen due to mixing opioids with other drugs, which is a common practice. Naloxone can save a life in a best scenario however; this is also the fact that it do nothing in worst case scenario.
Is naloxone dangerous?
Naloxone seldom shows rare and severe side effects. Opioid withdrawal is the most common side effect because naloxone removes the opioids from their receptors in the brain. The strength of a person’s dependency and higher doses of naloxone increases the risk of withdrawal symptoms. Aches, irritability, sweating, runny nose, diarrhea, nausea, and vomiting are the most common symptoms of opioid withdrawal.
Lung and heart problems, brain damage caused by prolonged lack of oxygen, and eventually, death are some potential complications of the opioid overdose which are quite alarming. In order to restore breathing, and reducing the risk of outcomes, naloxone should be given.
Will naloxone make you high?
The main and only effect of naloxone is to reverse the effect of opioids. Therefore naloxone cannot make you high. An injection of naloxone will acts as an injection of water if you are not taking opioids. Naloxone does not carry any risk of dependency or abuse.
Can you overdose on buprenorphine? Will naloxone stop such an overdose?
Buprenorphine is an opioid substitute treatment and one can get high on Buprenorphine. As compare to other opioids, there are lesser chances of overdose of this medication. Buprenorphine overdose mainly done with combination of sedatives, benzodiazepenes, or neuroleptics and it also involves the intravenous injection administration. Naloxone is not so effective in case of Buprenorphine overdose.
Naloxone injection should be given in a hospital to a health clinic, and it should be infused slowly and continuously in order to get the best results. A small number of overdoses cases have been reported with Buprenorphine. A sharp reduction in overdose fatalities is seen in countries such as France where Buprenorphine is readily available to treat opioid addiction.
Will naloxone work even if someone has previously used it?
Yes. You cannot develop tolerance to naloxone, so it can be used in every opioid overdose situation no matter how many times a person has overdosed in the past. People may respond to naloxone differently each time but this is often more likely due to how old the naloxone is, how it has been stored, what type of drugs the person took and in what dose or combination.
Is naloxone the same as naltrexone?
No, Naloxone is different from naltrexone in a way that naltrexone lasts longer than naloxone, usually 24 hours longer. Naltrexone is used in the treatment of the opioid or alcohol dependence. In the treatment of drug dependence, naloxone is sometimes used in combination of Buprenorphine. The combination of naloxone and buprenorphine is also available with the brand name “Suboxone”.
Can naloxone be safely used if it is expired?
Just like all other medicines, naloxone also loses its potency over a period of time. It may also lose its efficacy under the impact of too much heat or cold or even exposure to sunlight. Expired naloxone will not work as new and unexpired naloxone and also it will not show any side effects post expiry. Patients should exchange the old and expired naloxone with the new supply.
In the case, when a patient who is already had an overdose of opioid, given the expired naloxone, it will not show any effect in such case. The doctor may even have to increase the dose beyond the normal dose of naloxone in order to achieve the desired results. The victim should be monitored carefully and other evidence-based approaches, such as rescue breathing, should be used until the person revives or additional medical help arrives.
Proper storage measures should be considered in order to maintain the desired potency of naloxone. It should be stored in a dark and dry place.
Are there other ways to use naloxone besides injecting it?
Naloxone is also available in nasal spray form; however it is available in injectables form in many countries. Naloxone nasal spray is a formulation which contain concentrated amount of naloxone but unfortunately it is very expensive as compare to injectables form and is not readily available in many countries. Never try to pour the naloxone in patient’s mouth or nose as it can be extremely dangerous and can be entered into their lungs.
Can naloxone cause seizures?
In the absence of opioids, naloxone has almost no effects. It can cause sweating, nausea, vomiting, restlessness, flushing, and headache in people with opioids in their systems. In rare cases, naloxone has been shown to cause heart rhythm changes, seizures, and pulmonary edema as side effects.
What is the most important information I should know about naloxone (Narcan)?
You should not use this medication if you are allergic to it. In case you are hypersensitive to this drug and you are aware of this thing, Make sure that your doctor knows it. Even if you are pregnant or breast feeding, consult your doctor before taking it. Even after administration, make sure that your doctor knows that you have received this medication already.
Naloxone can alter your thinking or reaction process, so you should be careful while driving or doing anything that requires activeness. Naloxone can also reverse the effect of the narcotic pain medications, therefore be careful while taking pain killer medications along with Naloxone. Side effects of naloxone can be increased by drinking alcohol.
Can patients with cardiovascular disorders take naloxone?
Patients with cardiovascular disease, pulmonary edema, hypotension, ventricular arrhythmia, and hypertension should administer naloxone with caution. Also in patients with existing cardiovascular disorders it should be monitor for hypotension, hypertension, tachycardia or fibrillation, and pulmonary edema. Cardiovascular status and its clinical monitoring should be done in order to avoid any future consequence.
Can patients with liver disease take Naloxone?
In patients with Liver disease, the safety of the medication naloxone has not been established. Proper precaution is mandatory when giving naloxone to the patients with liver disease.
Can patients with renal disease take Naloxone?
Naloxone efficacy and effectiveness also not been established in patient with renal insufficiency or failure. If necessary to administer, it should be used with proper caution.
Can patients with septic shock take Naloxone?
In case of patient who suffered from a septic shock, Naloxone is observed to produce a rise in blood pressure which may lasts for several hours. However,, the patient survival has not been seen with the pressor response (Increase in blood pressure by constricting the vessels) of naloxone.
In some studies, treatment with naloxone in the setting of septic shock has been associated with adverse effects, including agitation, nausea and vomiting, pulmonary edema, hypotension, cardiac arrhythmias, and seizures. Therefore the use of naloxone in septic shock should be done with proper caution mainly in patients who already received opioid therapy previously or in patients who have underlying pain.
Should a patient with high blood pressure take Naloxone?
In patients with preexisting cardiovascular disorders, the naloxone therapy should be monitored closely for hypotension, hypertension, ventricular tachycardia or fibrillation, and pulmonary edema in an appropriate healthcare setting. Clinical monitoring of cardiovascular status is recommended.
What are withdrawal effects that are associated with Naloxone use?
Withdrawal reaction precipitated, and an abrupt reversal of narcotic depression may result in
- nausea, vomiting, sweating, tachycardia, increased blood pressure and tremulousness
- Cardiac arrest
- Ventricular fibrillation
- Dyspnea
- Pulmonary edema
- Abdominal cramps
- Diarrhea
- Cardiac arrest
- Hypertension
- Hypotension
- Ventricular tachycardia
- Paresthesia
- Restlessness
- Shivering
- Tonic-clonic seizures
- Yawning
- Diaphoresis
- Piloerection
- Hot flash
- Myalgia
- Tremor
- Weakness
- Rhinorrhea
- Sneezing
Can I take Paracetamol after naloxone?
There are no specific interactions found when naloxone is given with Paracetamol. But it does not necessarily means that there is no interaction exists between the two. Therefore you should always consult your doctor first before taking any medication.
What common medications interact with Naloxone?
Common:
- Naldemedine
- Naloxegol
Monitor closely:
- Buprenorphine
- Buprenorphine buccal
Minor:
- Alfentanil
- Belladonna and opium
- Butorphanol
- Codeine
- Dextromoramide
- Diamorphine
- Difenoxin hcl
- Diphenoxylate hcl
- Dipipanone
- Elvitegravir
- Hydrocodone
- Hydromorphone
- Levorphanol
- Meperidine
- Methadone
- Morphine
- Nalbuphine
- Opium tincture
- Oxycodone
- Oxymorphone
- Papaveretum
- Pentazocine
- Sufentanil
- Tapentadol
- Tramadol
What are the cautions needed for administration of Naloxone?
Naloxone should be used with caution in patients suffering from cardiovascular diseases or in patients who are taking medicines with cardiovascular effects, also in the patients who have a history of seizures. One should avoid the use of naloxone in treatment of meperidine-induced seizures.
One should observe the patients closely in patient who have administered long acting or partial agonist opioid as the chances of recurrence of respiratory depression are quite high. Patient should be monitored until there is no risk of recurrent respiratory or CNS depression. In the case of surgery, one should avoid excessive dosages of naloxone after use of opioids.
After surgery, an abrupt reversal of symptoms may occur and can cause nausea, vomiting, sweating, seizures, hypertension, and tachycardia and other cardiovascular events (pulmonary edema, arrhythmias) can also occur.
Auto-injector: (EVZIO)
When administered in infants of less than one year of age, you should monitor the site for residual needle parts and signs of infection at injection site.
Opioid withdrawal:
- Naloxone should be used with caution in patients, dependent on opioids, as naloxone can precipitate the abstinence syndrome.
- An abstinence syndrome is characterized by body aches, diarrhea, tachycardia, fever, runny nose, sneezing, pilo erection, sweating, yawning, nausea or vomiting, nervousness, restlessness, or irritability, shivering or trembling, abdominal cramps, weakness, and hypertension
- If left untreated or not recognized at time in neonates, it may prove life-threatening. The opioid withdrawal in neonates is characterized by convulsions, excessive crying, and hyperactive reflexes.
Use of naloxone in pregnancy & lactation
Pregnancy category: C is given for the naloxone administration, which means it should be used with caution and only if benefits outweigh risks. This category also stated that naloxone has been used for animal studies where it showed the risk and human studies not available for this medication.
Lactation: Not known if distributed in milk; use caution
Naloxone and droperidol
Extreme caution is needed in case of concurrent administration of droperidol with agents like naloxone. In order to achieve the desired effect the dose of droperidol should be titrated.
Because drugs like droperidol shows prolonged interval in QT wave, the routine vital sign and ECG is recommended. Patients should be closely monitored for excessive or prolonged CNS or respiratory depression, when droperidol is given in combination with the medication like naloxone (which can cause respiratory depression).
Activities that require mental alertness and motor coordination should be avoided by the ambulatory patients, and doctor should make them aware about the activity of such patients. Such patients should notify the prolonged CNS effects of this medication to the doctor.
Naloxone and fentanyl
This warning does not apply to the naloxone component in non-injectable formulations of naloxone-containing combination medicines. Naloxone reverses the action of opiates as it is an antagonist. When opiates are being abused the naloxone cause the reversal of opioids effects. Withdrawal symptoms can be noticed in patients who abuse opioids.
Narcan also works on the fentanyl overdoses, but it may need several doses to achieve the desired effect which depend upon potency of the opioid administered. As naloxone is a medication that does not work on the drugs which are not opioids. A sudden reversal of postoperative opioid effects can result in hypotension, ventricular tachycardia and fibrillation, pulmonary edema, cardiac arrest, encephalopathy, and death.
The changes in the vital signs such as nausea, vomiting, diarrhea, aches, fever, runny nose, sneezing, nervousness, irritability, shivering, and abdominal cramps should be monitored in patients who are receiving the naloxone injection.
Naloxone and codeine
This warning does not apply to the naloxone component in non-injectable formulations of naloxone-containing combination medicines. Naloxone injection is an antagonist that will reverse the actions of opiates. Effect of naloxone and reversal of opioids can occur only of the drug abused is opioid clinically.
A sudden reversal of postoperative opioid effects can result in hypotension, ventricular tachycardia and fibrillation, pulmonary edema, cardiac arrest, encephalopathy, and death. The changes in the vital signs such as nausea, vomiting, diarrhea, aches, fever, runny nose, sneezing, nervousness, irritability, shivering, and abdominal cramps should be monitored in patients who are receiving the naloxone injection.
Naloxone and Oxycodone
One should not administer the naloxone and oxycodone altogether, because naloxone can reverse the action if oxycodone. This condition is applied only if naloxone is given in injectable form. You may experience withdrawal symptoms if you are physically dependent on opioids. This can cause nausea, vomiting, diarrhea, aches, fever, runny nose, sneezing, nervousness, irritability, shivering, and abdominal cramps.
In case of any concerns or questions, contact your healthcare provider. A dose adjustment may be needed or in order to check the safety of concurrent administration of both drugs, the special test should be done. You should always let your doctor know if taking any herbs, vitamins or medications. You should also not stop taking any medication without prior consent of your doctor.
Naloxone and morphine
This warning does not apply to the naloxone component in non-injectable formulations of naloxone-containing combination medicines. Naloxone injection is an antagonist that will reverse the actions of opiates. Effect of naloxone and reversal of opioids can occur only of the drug abused is opioid clinically.
A sudden reversal of postoperative opioid effects can result in hypotension, ventricular tachycardia and fibrillation, pulmonary edema, cardiac arrest, encephalopathy, and death. The changes in the vital signs such as nausea, vomiting, diarrhea, aches, fever, runny nose, sneezing, nervousness, irritability, shivering, and abdominal cramps should be monitored in patients who are receiving the naloxone injection.
Can diazepam be given with naloxone?
There are no specific interactions found when naloxone is observed in naloxone with valium (Diazepam) concurrent administration. But it does not necessarily means that there is no interaction exists between the two. Therefore you should always consult your doctor first before taking any medication.
“What happens if you take hydrocodone and oxycodone at the same time?”
“How long after taking valium can I take xanax?“