Contents
- What is Paroxetine?
- Paroxetine molecular formula, weight, chemical name, drug class
- Why is Paroxetine medicine prescribed?
- How does Paroxetine work in the body?
- Paroxetine brand names
- Paroxetine FDA approved indications
- Paroxetine off-label use
- How must Paroxetine be taken?
- Paroxetine dosage for different indications
- Dose of Paroxetine in pregnancy
- Dose of Paroxetine in elderly patients suffering from renal or hepatic impairment
- Discontinuation of treatment with Paroxetine
- What happens if a dose of Paroxetine is missed?
- What happens if I overdose Paroxetine?
- Paroxetine side effects
- Paroxetine pharmacokinetics
- Warnings and precautions of Paroxetine
- Can Paroxetine cause risk of suicide?
- How Paroxetine affects sleep?
- Can Paroxetine cause bipolar disorder?
- Can Paroxetine cause Serotonin Syndrome?
- Can Paroxetine cause Angle-Closure Glaucoma?
- Can Paroxetine be used in pregnancy?
- Can Paroxetine be used during breastfeeding?
- Can Paroxetine be used in renal and liver disease?
- Can Paroxetine be used in elderly patients?
- Paroxetine and weight gain
- Can Paroxetine causes the activation of Mania/Hypomania
- Can Paroxetine cause seizures?
- Can Paroxetine causes akathisia?
- Can Paroxetine causes hyponatremia?
- Can Paroxetine causes abnormal bleeding
- Can Paroxetine cause fracture of the bones?
- Can I take Paroxetine with Tryptophan?
- Can I take Paroxetine with Monoamine Oxidase Inhibitors?
- Can I take Paroxetine with Pimozide?
- Can I take Paroxetine with serotonergic drugs?
- Can I take Paroxetine with Warfarin?
- Can I take Paroxetine with triptans?
- Can I take Paroxetine with drugs affecting hepatic metabolism?
- Can I take Paroxetine with Cimetidine?
- Can I take Paroxetine with Phenobarbital?
- Can I take Paroxetine with Phenytoin?
- Can I take Paroxetine with Tricyclic antidepressants?
- Can I take Paroxetine with drugs bound to plasma protein?
- Can I take Paroxetine with drugs that interfere with hemostasis like Aspirin, NSAIDs, and Warfarin?
- Can I take Paroxetine with alcohol?
- Can I take Paroxetine with Lithium?
- Can I take Paroxetine with Digoxin?
- Can I take Paroxetine with Procyclidine?
- Can I take Paroxetine with Theophylline?
- Can I take Paroxetine with Fosamprenavir/ritonavir?
What is Paroxetine?
Paroxetine is a generic name for a drug that belongs to the category of antidepressants. It is known as SSRIs (Selective serotonin reuptake inhibitors). It is effective to the patients that are suffering from anxiety, depression and other disorder. It is used to treat post- obsessive compulsive disorder, traumatic stress, depression, and anxiety. Paroxetine is also effective in the treatment of hot flashes during menopause.
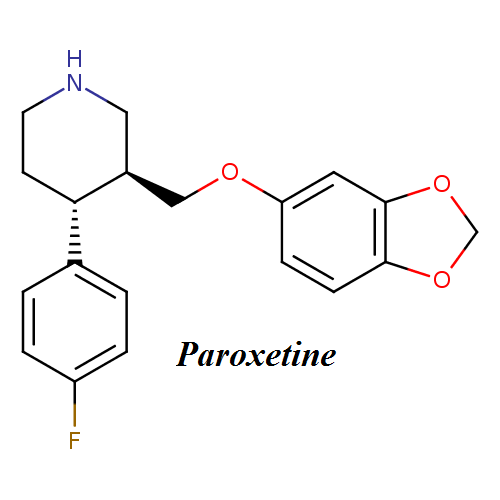
Paroxetine molecular formula, weight, chemical name, drug class
Molecular weight– 329,3 g/mol
Chemical name – (-)-(3S,4R)-4-(P-Fluorophenyl)-3-((3,4-(methylenedioxy)phenoxy)methyl)piperidine
This compound belongs to the class of organic compounds known as phenylpiperidines. These are compounds containing a phenylpiperidine skeleton, which consists of a piperidine bound to a phenyl group.
Chemical or Molecular Formula– C19H20FNO3
Paroxetine pharmacological class drug class– SSRIs (Selective serotonin reuptake inhibitors)
Paroxetine molecular formula:
Why is Paroxetine medicine prescribed?
This medicine is prescribed to treat the following ailments:
-
Major Depression
The efficacy of Paroxetine was established in the controlled trials. In this trial, the patients were diagnosed with the major depressive disorder. This state of depression affects the daily functioning. It has the following symptoms like change in appetite, sleep, and loss of interest in daily activities.
It can also cause fatigue, slowed thinking, impair concentration, feeling of guilt and agitation. It can also lead to thinking of suicide. The efficiency of Paroxetine was observed for one year in the placebo controlled trial.
-
Obsessive Compulsive Disorder
Paroxetine is indicated for the treating obsessions & compulsions in patients with OCD. The compulsions and obsessions cause distress and interfere with social or office or daily activity. The efficacy of Paroxetine was observed in 12-week trials. It was carried in the patients suffering from OCD.
OCD is characterized by persistent and recurrent ideas, impulses, thoughts, or images (obsessions). These actions are repetitive and intentional behaviors (compulsions) that are recognized as unreasonable or excessive. The long-term maintenance efficacy was observed in a 6-month trial. In this trial, patients given paroxetine showed a lower relapse rate as compared to patients who are on placebo.
-
Panic Disorder
It is indicated to treat panic disorder without or with agoraphobia. It is characterized by unexpected panic attacks. The consequences of these attacks and change in behavior are also the area of concern. The efficacy was observed for 10-to 12-week clinical trials in the patients suffering from panic disorders.
The symptoms of panic disorders are palpitations, accelerated heart rate, pounding heart, sweating, shaking, shortness of breath or smothering, choking and chest pain or discomfort. It can also result in abdominal distress, nausea, lightheaded, unsteady, and fainting.
-
Social Anxiety Disorder
Paroxetine is indicated for the treating social anxiety disorder known as social phobia. It is characterized by persistent fear of social or performance situations. The exposure to the unfamiliar situation can provoke anxiety and increases the intensity of a panic attack.
The distress and anxiety have a huge impact on person’s normal routine, academic functioning, and social relations. The efficacy of Paroxetine was observed in 12-week trials in the patients suffering from social anxiety disorder.
-
Generalized Anxiety Disorder
Paroxetine is used to treat Generalized Anxiety Disorder. The efficacy of Paroxetine was observed in 8-week placebo-controlled trials in the adults suffering from GAD. The effect has not been known in children.
It is characterized by worry and excessive anxiety that is persistent for minimum 6 months. The symptoms are fatigue, difficulty in concentration, Restlessness, mind going blank, muscle tension, irritability and disturbance in sleep. The efficacy of paroxetine has been studied in an 8-week acute clinical trial in the patient suffering from generalized anxiety disorder.
-
Posttraumatic Stress Disorder
Paroxetine is used to treat Posttraumatic Stress Disorder. The efficacy was studied in 12-week placebo-controlled trials in the adults suffering from this ailment. It can occur due to exposure to an event that involves actual death or serious injury. The symptoms are psychological distress, flashbacks, avoidance of situations, numbing, lost interest in significant activities and dreams.
Other symptoms are sleep disturbance, outbursts of anger, irritability and impaired concentration. The symptoms may be present at least a month. It can adversely affect your social and professional life.
How does Paroxetine work in the body?
Paroxetine is a potent drug. It is a selective inhibitor of serotonin reuptake. It inhibits the reuptake of serotonin and enhances serotonergic neurotransmission. It increases the activity of paroxetine at synaptic receptors. It also potentiates the action of 5-HT in the CNS.
Paroxetine brand names
Paroxetine is known under following Brand names on the market: Paxil CR, Brisdelle, Paxil, Pexeva

Paroxetine FDA approved indications
FDA approved indications for paroxetine are:
- Generalized Anxiety Disorder (GAD)
- Irritable Bowel Syndrome (IBS)
- Major Depressive Disorder (MDD)
- Obsessive-Compulsive Disorder (OCD)
- Panic Disorders
- Post-Traumatic Stress Disorder (PTSD)
- Premenstrual Dysphoric Disorder
- Social Anxiety Disorder (SAD)
- Vasomotor Symptoms
Brisdelle, which consists of paroxetine mesylate is indicated for the treatment of moderate to severe vasomotor symptoms (like hot flashes) associated with menopause.
Paroxetine off-label use
Unlabeled indications of paroxetine include:
- Eating disorders
- Impulse control disorders
- Vasomotor symptoms of menopause
- Obsessive-compulsive disorder (OCD) in children
- Mild dementia-associated agitation in nonpsychotic individuals.
How must Paroxetine be taken?
- You must take paroxetine as prescribed by the doctor. You must follow all the directions given by the doctor. Your doctor can change your dose. You are advised not to take this medicine in larger or smaller amounts.
- Do not chew, crush, or break an extended-release tablet. You must swallow it.
- Shake oral suspension before taking it. Measure the liquid medicine with dosing syringe or medicine cup.
- It can take 4 weeks to improve your symptoms. Use the medicine as directed by your physician.
- Do not stop taking paroxetine else you could suffer from withdrawal symptoms.
- You must consult your doctor if you want to stop using paroxetine.
- Store paroxetine away from moisture, light, and heat. Store it at room temperature.
Before taking this medicine you must take into considerations the following things.
- Do not use this drug if you are allergic to it.
- Avoid taking this drug if you are also taking thioridazine or pimozide
- Do not use MAO inhibitor 14 days before and after you start taking Paroxetine. The dangerous drug interaction can occur.
Tell your doctor if you have
- Seizures or epilepsy
- Heart disease, history of stroke and high blood pressure
- Kidney or liver disease
- Low levels of sodium in the blood
- Bleeding or blood clotting
- Glaucoma
- If you are pregnant, planning to conceive.
- If you are a nursing mother as paroxetine passes into the breast milk.
Paroxetine dosage for different indications
- Major Depressive Disorder
Initial Dose- Paroxetine must be given as a single dose daily. It can be given with or without food in the morning. Recommended initial dose is 20 mg/day. The usual range of the dose is 20 to 50 mg/day. The effect of the treatment can be delayed. The patients who don’t respond to 20-mg dose, the dose is increased to a maximum of 50 mg/day.
Maintenance Dose- The treatment of these acute episodes may require several months. You must consult with your doctor. The systematic evaluation of the efficacy of Paroxetine indicates that the efficacy can be maintained up to 1 year with doses of about 30 mg.
- Obsessive Compulsive Disorder
Initial Dose- Paroxetine must be given as a single dose daily with or without food in the morning. The recommended dose of paroxetine for treating OCD is 40 mg daily. The patients must be started from 20 mg/day and the dose can be increased to10-mg/day. The changes in dose must occur at the intervals of at least a week. Patients were given a dose in a range of 20 – 60 mg/day in the clinical trials. The effectiveness of Paroxetine was seen in the case of OCD. The maximum dose must not exceed 60 mg/day.
Maintenance Dose- The maintenance dose was demonstrated in a 6-month trial. It is a chronic condition that requires the maintenance dose. The adjustments in dose must be made. It must be started from the lowest effective dosage. The patients must be assessed from time to time.
- Panic Disorder
Initial Dose- Paroxetine must be given as a single dose daily with or without food in the morning. The target dose that is given in treating panic disorder is 40 mg/day. The patients must start from10 mg/day. The changes in dose may be increased by 10-mg/day. The increment of the dose must be done at the intervals of at least a week. Patients can be given the dose in a range of 10 – 60 mg/day. The maximum dosage must not exceed more than 60 mg/day.
Maintenance Dose- The maintenance dose was studied in a 3-month trial. In this trial, the patients suffering from panic disorder were given paroxetine to determine the efficacy of the dose. It is a chronic condition that requires a long term maintenance dose according to the severity of the disease. The dose adjustments must start from the lowest effective dosage. Patients must be assessed from time to time.
- Social Anxiety Disorder
Initial Dosage- Paroxetine must be given as a single dose daily with or without food in the morning. The recommended dose is 20 mg/day. The effectiveness of Paroxetine was studied in the clinical trial. The dose of the patients is evaluated between 20 to 60 mg/day. The safety of Paroxetine was evaluated in patients at doses of up to 60 mg/day.
Maintenance Therapy– The efficiency of Paroxetine for maintenance dose was not demonstrated beyond 12 weeks in the patients that were suffering from social anxiety disorder. It is a chronic condition. The dose adjustments can be made starting from the lowest effective dose. The patients must be periodically assessed.
- Generalized Anxiety Disorder
Initial Dosage- Paroxetine must be given as a single dose daily with or without food in the morning. The effectiveness of Paroxetine was studied in the clinical trial the range of 20 to 50 mg/day. The recommended dose is 20 mg/day. The dose adjustments can be started from 10 mg/day increment and at the interval of a week.
Maintenance Therapy– The evaluation of Paroxetine was done for the period of 24 weeks in patients that were suffering from Generalized Anxiety Disorder. The patients must be assessed to determine the effectiveness of the maintenance treatment.
- Posttraumatic Stress Disorder
Initial Dosage- Paroxetine must be given as a single dose daily with or without food in the morning. The recommended dose is 20 mg/day. The effectiveness of Paroxetine was studied in the patients in the dose range of 20 to 50 mg/day. The changes in doses must be done from 10 mg/day increment and at the interval of a week.
Maintenance Therapy- The efficacy of Paroxetine was studied for 12 weeks of dose. The PTSD is a chronic condition. The dose adjustments must be made as per the lowest effective dose. The patients must be assessed on the regular basis.
Dose of Paroxetine in pregnancy
It was found that the neonates, when exposed to Paroxetine developed complications. The pregnant women were given respiratory support and prolong hospitalization. If you are treating pregnant women with this drug during the 3rd trimester, then the physician must be aware of the potential risk with this drug.
Dose of Paroxetine in elderly patients suffering from renal or hepatic impairment
The recommended dose is 10 mg/day for elderly patients that are suffering from severe hepatic or renal impairment. The dose must not exceed 40 mg/day.
Discontinuation of treatment with Paroxetine
The symptoms that are associated with discontinuation of Paroxetine are observed. The patients must be observed with the symptoms of discontinuation of Paroxetine. It is suggested for the gradual reduction in the dose. We will not recommend the abrupt cessation of Paroxetine.
What happens if a dose of Paroxetine is missed?
You must take the missed dose soon. You can skip the missed dose if it is the time for the next dose. You are advised not to take extra medicine.
What happens if I overdose Paroxetine?
In the case of overdose, consult your doctor immediately. The overdose of paroxetine can be fatal.
Paroxetine overdose symptoms may include:
- Sleepiness or extreme fatigue
- Coma
- Involuntary shaking or twitching
- Fast, pounding, irregular, or slow heartbeat
- Confusion
- Nausea
- Vomiting
- Dizziness
- Seizures
- Fainting
- Blurry vision
- Unusual bruising or bleeding
- Loss of energy or appetite
- Pain in the upper right part of the stomach
- Flu-like symptoms
- Yellowing of the skin and eyes (jaundice)
- Aggressive behavior
- Muscle pain, stiffness, or weakness
- Dark red or brown urine
- Troubling urinating
- Diarrhea
- Feeling unusually excited
- Sweating
- Fever
- Trouble walking
Paroxetine side effects
The signs of an allergic reaction are skin rash, swelling of face, tongue, lips & throat and difficulty in breathing. You have other symptoms like changes in mood or behavior, panic attacks, anxiety, trouble in sleeping, hostile, hostile and aggressive.
Contact your doctor if you have following side effects-
- The flood of Thoughts, more talkative, decreased sleep, feelings of extreme sadness or happiness.
- Blurred vision, eye pain, eye swelling, and tunnel vision
- Tenderness or bone pain, swelling and bruising
- Changes in appetite and weight
- Bruising, coughing up blood and unusual bleeding
- High serotonin level– Hallucinations, fast heart rate, nausea, diarrhea. overactive reflexes and loss of coordination
- Low levels of sodium- Headache, severe weakness, slurred speech and confusion
- The severe reaction of nervous system- rigid) muscles, sweating, high fever, confusion, uneven heartbeats, and fainting.
- Severe skin reaction– swelling in your face or tongue, burning in eyes, sore throat, blistering and peeling
- Dizziness, weakness and drowsiness
- Shaking, sweating, and anxiety
- Constipation and loss of appetite
- Yawning and dry mouth
Paroxetine pharmacokinetics
Absorption- It gets absorbed slowly but completely. The oral bioavailability is low due to the first-pass metabolism. The peak concentrations of mesylate salt reached at 6 hours. The steady C max is 13.10 ng/mL. It generally has non-linear pharmacokinetics because of CYP2D6.
The volume of distribution- The volume of distribution is found as 3.1-28 L/kg in animal studies. It gets distributed throughout the body. It also gets distributed in the central nervous system. Only 1% remain in the plasma.
Protein Binding- 95% bound to plasma proteins.
Metabolism- Paroxetine gets metabolized in the liver. The metabolites that are polar and conjugated products gets readily eliminated by the body. The metabolites are sulfate conjugate and glucuronic acid. This drug is metabolized by P450 -CYP 2D6.
Route of Elimination- 64% of 30 mg oral solution is excreted in the urine – 2% as parent compound & 62% as metabolites. Approximately 36% of the dose gets excreted in the feces.
Half- Life– 21-24 hours
Warnings and precautions of Paroxetine
- Don’t take alcohol with Paroxetine as it can cause side effects.
- You must consult your doctor if you are taking NSAID for pain, fever, arthritis, fever, and swelling. Some of the drugs are ibuprofen, aspirin, celecoxib, naproxen, diclofenac, meloxicam, indomethacin, and others. If you use paroxetine with NSAID may cause bruising or bleeding.
- Paroxetine can impair your thinking. Be careful in the case of driving or doing any activity that involves concentration.
Can Paroxetine cause risk of suicide?
The patients suffering from the major depressive disorder can experience worsening of depression and an idea of suicide or unusual change in behavior. Suicide is the foremost symptom of severe psychiatric disorders.
It is been the concern of people that antidepressants may cause worsening of depression. It can also lead to the emergence of suicide. The placebo-controlled trials was carried out in antidepressant drugs. It showed that drugs increase the risk of suicide in adults, children, and adolescents in the patients that were suffering from MDD.
The patients that are treated with antidepressants like Paroxetine must be monitored for the tendency of suicide, unusual changes in behavior and worsening of depression. These signs can be seen during the starting of the therapy or the change in the dose.
If any patient is suffering from the suicidal tendency, then the treatment must be changed. In the case of discontinuation of the therapy it must be done under the guidance of the doctor. The patients on the treatment of paroxetine must have a look at the signs like agitation or irritability
How Paroxetine affects sleep?
Paroxetine, like other serotonin reuptake inhibitors (SSRIs), works on certain brain chemicals that interacts with sleep architecture. Specifically, these antidepressant drugs may delay the onset of REM (rapid eye movement) sleep which is essential in achieving a relaxing sleep.
It can also increase the chances of awakenings which can negatively impact the quality of sleep. Additionally, paroxetione has been associated with abnormal dreams and nightmares, especially when used for treatment of posttraumatic stress disorder and obsessive-compulsive disorder. This possible side effect can also affect patient’s sleep.
However, there are other factors that can contribute to insomnia. For instance, patients taking Paxil for depression may have insomnia as a symptom of the condition. Chemical imbalances in the brain can also be attributed to difficulty sleeping. Aside from depression, there other emotional conditions can likewise result in trouble falling asleep and staying asleep.
Because of the many contributing factors, it is quite difficult to know the actual cause of insomnia in patients taking Paxil.
Can Paroxetine cause bipolar disorder?
It is believed that treating bipolar disorder with Paroxetine can precipitate mixed or manic episode in the patient who is at the risk of bipolar disease. Before starting the treatment you must investigate that the patient is at the risk of bipolar disorder. The doctor must ask for your psychiatric history that includes family history of suicide, depression, and bipolar disorder.
Can Paroxetine cause Serotonin Syndrome?
The development of a life-threatening serotonin syndrome has been reported with Paroxetine. The symptoms are hallucinations, agitation, delirium, flushing, tachycardia, dizziness, neuromuscular problems, and seizures.
The paroxetine must not be administered with MAOIs like methylene blue or linezolid. If paroxetine is taken with other serotonergic drugs, then be aware of the risk of serotonin syndrome. The treatment with Paroxetine and other serotonergic agents must be discontinued immediately.
Can Paroxetine cause Angle-Closure Glaucoma?
The pupillary dilation occurs after the use of antidepressant drugs like Paroxetine. It can trigger the angle closure attack in a person that has anatomically narrow angles.
Can Paroxetine be used in pregnancy?
Teratogenic Effects- The studies have shown that infants who are exposed to paroxetine in the first three months of pregnancy develop the risk of congenital and cardiovascular malformations. There were many studies that showed these risks.
- A study was done in Sweden in which infants were exposed to paroxetine during pregnancy. They were found to be at the risk of cardiovascular malformations. The risk of congenital malformations was not observed. The cardiac malformations like ventricular septal defects and atrial septal defects were found to be common.
- A cohort study was done in the United States. The 5,956 infants of mothers were given paroxetine during the first trimester. It resulted in the increased risk of cardiovascular malformations for paroxetine of about 1.5%. This study also showed an increased risk of congenital malformations of about 4%.
- Two large studies were conducted. They were >9,000 birth defect cases and >4,000. The maternal use of paroxetine during first three months of pregnancy caused the increased risk of right ventricular outflow tract obstructions.
Non-teratogenic Effects- Neonates were exposed to Paroxetine in the last trimester have been reported with respiratory support, prolong hospitalization and tube feeding. The clinical studies have shown symptoms like respiratory distress, seizures, temperature instability, and difficulty in feeding.
Other symptoms are vomiting, hypoglycemia, tremor, and irritability. The Infants that were exposed paroxetine in pregnancy have the increased risk of pulmonary hypertension in the newborn. It occurs in 1 – 2 per 1,000 live births and is associated with morbidity and mortality.
Can Paroxetine be used during breastfeeding?
Because of the low levels of paroxetine in breastmilk, amounts ingested by the infant are small and paroxetine has not been detected in the serum of most infants tested. Occasional mild side effects have been reported, especially in the infants of mothers who took paroxetine during the third trimester of pregnancy, but the contribution of the drug in breastmilk is not clear.
Most authoritative reviewers consider paroxetine one of the preferred antidepressants during breastfeeding. Occasional mild side effects such as insomnia, restlessness and increased crying have ben reported in breastfed infants.
Mothers taking an SSRI during pregnancy and postpartum may have more difficulty breastfeeding and may need additional breastfeeding support. Breastfed infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation than formula-fed infants.
Can Paroxetine be used in renal and liver disease?
The plasma concentrations of paroxetine increases in the patients suffering from renal and hepatic impairment. The plasma concentration of paroxetine in the patients with creatinine clearance below 30 mL/min. was 4 times greater than normal people.
The patients with creatinine clearance of 30 – 60 mL/min. and hepatic functional impairment had 2‑fold increase in plasma concentrations of paroxetine. The initial dosage must be reduced in patients with severe renal or hepatic impairment.
Can Paroxetine be used in elderly patients?
The multiple‑dose study was conducted in the elderly at doses of 20, 30, and 40 mg. The Cmin concentrations were 70% to 80% greater. The initial dosage in the elderly must be reduced.
Paroxetine and weight gain
Like most of these antidepressant drugs,paroxetine is commonly thought to be the cause of unexpected weight gain in patients taking the drug. In clinical studies conducted before paroxetine was approved, a few patients reported weight gain as a side effect. However, every individual responds differently to certain medication. Some may gain weight while others would report weight loss.
Before any medication is approved, it undergoes extensive clinical evaluation where it is given to thousands of participants. Data is then gathered and compared to a group of people who did not take the drug. These studies document the side effects caused by the medication. Side effects are then categorized either as common side effects (reported by more than 1 percent of users) and rare side effects (reported by less than 1 percent of users).
Studies show that weight gain occurs in more than 1 percent of users, although the exact percentage is not known. These studies on Paxil reflect other studies conducted on other antidepressants which show that up to 25% of people who use antidepressant medications report weight gain.
Recent findings further reveal that patients who use paorxetine gain more weight in just short time (six months) compared to other antidepressants, like bupropion (Wellbutrin), nefazodone (Serzone), and venlafaxine (Effexor). Patients often report an increase in weight, 10 pounds or more.
Although weight gain may be noticed after initiating treatment, the medication is not always the direct cause. There are a number of factors that can contribute to weight gain while taking antidepressant therapy, including paroxetine.
For instance, some patients may engage in overeating as a symptom of depression which can cause weight gain. Poor diet, particularly craving for unhealthy foods, along with inactivity is also very common among people who are suffering from emotional conditions. These can all contribute to weight gain.
Can Paroxetine causes the activation of Mania/Hypomania
During the premarketing testing it was detected that the mania occurred in approximately 1.0% of unipolar patients treated with Paroxetine compared to 1.1% of active‑control and 0.3% of placebo‑treated unipolar patients. In a subset of patients classified as bipolar, the rate of manic episodes was 2.2% for Paroxetine and 11.6% for the combined active‑control groups. As with all drugs effective in the treatment of major depressive disorder, Paroxetine should be used cautiously in patients with a history of mania.
Can Paroxetine cause seizures?
During the premarketing testing, the 0.1% of seizures were reported in the patients who were treated with Paroxetine. Paroxetine must be cautiously given in patient have the history of seizures. It must be discontinued in the patient who develops seizures.
Can Paroxetine causes akathisia?
The administration of paroxetine can cause akathisia that is defined as restlessness and psychomotor agitation. It causes an inability to sit or stand still. This can occur within the first few weeks of the administration of paroxetine.
Can Paroxetine causes hyponatremia?
Hyponatremia may occur as a result of administration of Paroxetine. The cases of low serum sodium have been reported. Elderly patients are at the greater risk of developing hypernatremia. The patients who are taking diuretics also are at the greater risk of Hyponatremia. The discontinuation of Paroxetine must be considered in patients with symptomatic hyponatremia.
The signs and symptoms of hyponatremia are headache, difficulty in concentrating, confusion, memory impairment, unsteadiness and weakness. The symptoms of severe cases of Hyponatremia are seizure, hallucination, respiratory arrest syncope, coma, and death.
Can Paroxetine causes abnormal bleeding
Paroxetine can increase the risk of bleeding. The cases were reported that have demonstrated the use of paroxetine that can result in the gastrointestinal bleeding. The bleeding events can result in hematomas, ecchymoses, epistaxis to life-threatening hemorrhages. Patients must be careful about the risk of bleeding with the use of paroxetine and aspirin and NSAIDs that affect coagulation.
Can Paroxetine cause fracture of the bones?
The epidemiological studies have demonstrated the risk of fracture with use of Paroxetine. The possibility of a fracture can be due to decreased bone mineral density in the patient that are taking paroxetine.
Can I take Paroxetine with Tryptophan?
The interaction occurs between paroxetine and tryptophan when they are administered together. The symptoms are nausea, headache, sweating, and dizziness are reported. The co-administration of both these drugs are not recommended.
Can I take Paroxetine with Monoamine Oxidase Inhibitors?
The use of MAOIs with Paroxetine within 14 days of stopping the treatment with Paroxetine is contraindicated as there is an increased risk of serotonin syndrome. Also, the use of Paroxetine within 14 days of stopping MAOI is contraindicated. Starting Paroxetine in the patient who is on the treatment of MAOIs is contraindicated as it results in increased risk of serotonin syndrome.
Can I take Paroxetine with Pimozide?
In the controlled study 60 mg of Paroxetine with 2 mg of pimozide was administered to the healthy volunteers. It resulted in the increase of AUC of 151% of Pimozide. The Cmax also increased to 62% as compared with pimozide administered alone. The increase of pimozide AUC and Cmax is because of CYP2D6 inhibitory features of paroxetine. The concomitant use of pimozide and Paroxetine is contraindicated
Can I take Paroxetine with serotonergic drugs?
You must be cautious when taking paroxetine with serotonergic drugs like triptans, fentanyl, lithium, amphetamines, and tramadol. The concomitant use of Paroxetine with MAOIs is contraindicated.
Can I take Paroxetine with Warfarin?
The preliminary data have suggested that there can be a pharmacodynamic interaction between paroxetine and warfarin. It can cause an increased bleeding diathesis. The warfarin and paroxetine must be taken with caution.
Can I take Paroxetine with triptans?
The concomitant use of Paroxetine with Triptan is warranted. The patients are advised to be under careful observation during the initiation of treatment and the changes in dose.
Can I take Paroxetine with drugs affecting hepatic metabolism?
The pharmacokinetics and metabolism of paroxetine are affected by the induction or inhibition of drug‑metabolizing enzymes.
Can I take Paroxetine with Cimetidine?
Cimetidine inhibits cytochrome P450 enzymes. In a clinical study, Paroxetine 30 mg was given for 4 weeks. It resulted in the increase of plasma concentrations of paroxetine by 50% during co-administration with cimetidine. Therefore, the caution must be taken while administering this two drug together.
Can I take Paroxetine with Phenobarbital?
Phenobarbital induces cytochrome P450. The oral 30-mg dose of Paroxetine was given with Phenobarbital of dose 100 mg daily for 14 days. The paroxetine AUC was reduced by 25% and T½ was reduced 38%, respectively compared to paroxetine taken alone. You must take paroxetine and phenobarbital under the guidance of a doctor.
Can I take Paroxetine with Phenytoin?
The 30-mg dose of Paroxetine was given with phenytoin of 300 mg for 14 days. It resulted in the decrease of AUC by 50% and T½ was reduced by 35% when compared to Paroxetine administered alone.
In another study, when the 300-mg dose of phenytoin was administered with paroxetine steady state of 30 mg for 14 days. It resulted in the decrease of phenytoin AUC by 12% compared to phenytoin when administered alone. You must be cautious when taking these two drugs together. You must take these drugs under the guidance of a doctor.
Can I take Paroxetine with Tricyclic antidepressants?
The caution must be taken while taking tricyclic antidepressants (TCAs) with Paroxetine. Paroxetine can inhibit TCA metabolism. TCA plasma concentrations need to be monitored carefully. The dose of TCA can be reduced if TCA is taken with Paroxetine.
Can I take Paroxetine with drugs bound to plasma protein?
Paroxetine gets bound to plasma protein. The administration of Paroxetine with another drug that bounds to the protein can cause increased free concentrations of another drug. It can result in adverse events.
Can I take Paroxetine with drugs that interfere with hemostasis like Aspirin, NSAIDs, and Warfarin?
Serotonin that is released by platelets plays an important role in the hemostasis. Many studies have shown that psychotropic drugs interfere with serotonin reuptake.
The occurrence of upper gastrointestinal bleeding has also been demonstrated. The use of NSAID or aspirin can increase the risk of bleeding. The increase in bleeding has also been reported when paroxetine is administered with warfarin. Patients receiving these drugs with paroxetine must be carefully monitored.
Can I take Paroxetine with alcohol?
The patients must be advised to avoid alcohol while taking Paroxetine.
It is believed that alcohol and paroxetine act on the same brain chemicals therefore should not be used together. Combining Paxil and alcohol may enhance the effects of alcohol, possibly causing an increase in symptoms of depression; affect motor skills; or impairment in thinking and judgment.
Although patients are advised to avoid alcohol while taking Paxil, consuming moderate amounts of alcohol is not expected to cause life-threatening side effects. Generally, some patients can safely drink moderate amounts of alcoholic beverages.
Depending on your condition, your healthcare provider may advise limiting your intake of alcohol to light to moderate amounts, and only if you already know the effects of Paxil on your body and if your condition is well-controlled. People who are taking other medications for depression should also consider drinking alcohol with extreme caution.
Can I take Paroxetine with Lithium?
The studies have shown that there is no pharmacokinetic interaction between Paroxetine and lithium. Due to serotonin syndrome you are advised to take Paroxetine with lithium.
Can I take Paroxetine with Digoxin?
The AUC of digoxin decreased by 15% when given with paroxetine. The administration of digoxin and paroxetine should be taken with caution.
Can I take Paroxetine with Procyclidine?
The dose of Paroxetine of 30 mg is given with Procyclidine of 5 mg. It resulted in the increase of AUC0-24 by 35%, Cmax by 37%, and Cmin by 67% compared to procyclidine alone. If the anticholinergic effects are observed then the dose of procyclidine must be reduced.
Can I take Paroxetine with Theophylline?
The Report of elevated theophylline levels with Paroxetine are reported. The theophylline levels must be monitored in the case of co- administration of both these drugs.
The simultaneous administration of paroxetine with fosamprenavir/ritonavir resulted in the decreased levels of paroxetine.