Contents
- What is leukocyte esterase?
- What is leukocyte esterase test in urine?
- How is leukocyte esterase test performed?
- How to prepare for the leukocute esterase test?
- Is leukocute esterase test uncomfortable?
- How to collect clean catch urine sample for leukocyte esterase test?
- What are urine test strips (dipsticks)?
- Urine test strips (dipsticks) test and detection of leukocytes
- Can leukocyte esterase test give false positive or negative results?
- The sensitivity for leukocyte esterase test
- Combur-test strips for leukocyte esterase test
- What may positive leukocyte esterase test indicate?
What is leukocyte esterase?
Leukocyte esterase (LE) is an esterase type of enzyme produced by leukocytes (white blood cells). Esterases are hydrolytic enzymes that hydrolyze (splits) esters compounds into the acid and an alcohol.
What is leukocyte esterase test in urine?
A leukocyte esterase test or LE test is a urine type of test (urinalyses) for detecting white blood cells and other abnormalities correlated with infection. This screening test is used to indicate urinary tract infection (UTI). Positive LE test results are clinically significant. The LE test is also used to screen for amniotic fluid infections and gonorrhea.
The combination of the urinary nitrite test with LE test provides an excellent screen for predicting a urinary tract infection. If urine sample is positive for both nitrate and leukocyte esterase tests then it should be cultured for pathogenic bacteria. These tests are indirect ways of detecting bacteria in the urine.
The LE test is often indicated to screen patients at high-risk for UTI, including elderly patients, pregnant women, school-age females, and individuals with a history of urinary tract infections. The other name for this test is WBC (white blood cell) esterase.
How is leukocyte esterase test performed?
For best results of LE test, clean-catch urine sample (described in further text) is preferred. The clean-catch urine sample is needed in order to prevent germs from the vagina or penis from getting into a urine sample.
To collect your urine properly, the health care provider will give you a special clean-catch kit that with a cleansing solution and sterile wipes. You will have to follow your doctor’s instructions carefully so that the results will be accurate.
After providing a urine sample, test should be performed right away. The provider uses a dipstick (described in further text) made with a color-sensitive pad. The color (for LE usually purple) of the dipstick changes indicated if you have leukocytes in the urine.
How to prepare for the leukocute esterase test?
There are no special actions needed to prepare for this test.
Is leukocute esterase test uncomfortable?
No it is not. The test only involves normal urination. There are no discomforts.
How to collect clean catch urine sample for leukocyte esterase test?
For best results, collect the sample when the urine has been in your bladder for 2 to 3 hours. You will use a special kit that your doctor gives you to collect the urine. It most likely looks like a cup with a lid and wipes. Wash your hands with soap and warm water before collecting the sample.
Instructions for correct clean catch urine sampling for women:
- Wash the area between the vaginas “lips” (labia). You may be given a special clean-catch kit with sterile wipes.
- Sit on the toilet with your legs spread apart. Use two fingers to spread open your labia.
- Use the first wipe to clean the inner folds of the labia then wipe from the front to the back.
- Use a second wipe to clean over the opening where urine comes out, just above the opening of the vagina
- Keeping your labia spread open, urinate a small volume into the toilet bowl, then stop the urine flow
- Hold the urine cup a few inches (or a few centimeters) from the urethra and urinate until the cup is about half full.
- You may finish urinating into the toilet bowl
Instructions for correct clean catch urine sampling for men:
- Urinate a small amount into the toilet bowl, and then stop the flow of urine.
- Then collect a sample of urine into the clean or sterile cup, until it is half full.
- You may finish urinating into the toilet bowl
Instructions for correct clean catch urine sampling for infants:
- You will be given a special pediatric/infant bag to collect the urine. It will be a plastic bag with a sticky strip on one end, made to fit over your baby’s genital area.
- If the collection is being taken from an infant, you may need extra collection bags.
- Wash the area well with soap and water, and dry. Open and place the bag on your infant.
- For boys, the entire penis can be placed in the bag.
- For girls, place the bag over the labia.
- You can put on a diaper over the bag.
- Check the baby often and remove the bag after the urine collects in it. Active infants may displace the bag, so you may need to make more than one attempt. Drain the urine into the container you were given and return it to the health care provider as directed.
After the sample is collected screw the lid tightly on the cup. Do not touch the inside of the cup or the lid. Return the sample to your healthcare provider. If you are at home, place the cup in a plastic bag and put the bag in the refrigerator until you take it to the lab or your provider’s office.
What are urine test strips (dipsticks)?
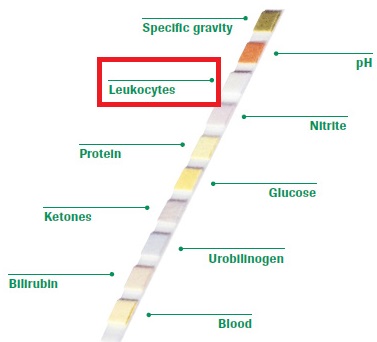
A urine test strip which is also known as dipstick is a routine diagnostic tool used to indicate pathological changes in a patient’s urine of a standard urinalysis.
A standard urine test strip usually has 10 different reagents/chemical pads which react with the urine by changing a color when dipped in, and then removed from a urine sample. The test can be read in as little as 60 to 120 seconds after dipping, although certain tests may need longer time.
Routine testing of the urine with strips is usually the first step in the diagnosis of a various diseases. Urine test strips can measure the presence of: proteins, hemoglobin, glucose, ketones, urobilinogen, bilirubin, acetone, nitrite and leucocytes as well as testing of specific gravity and pH or to test for infection by different organisms.
Urine test strips (dipsticks) test and detection of leukocytes
In a urine sample, 3 (occasionally 5) leukocytes per high power field (40X) are normal results. However, women might have somewhat higher results because of the vaginal contamination. Higher numbers of leukocytes indicate urinary infection.
The urine test strip test/dipsticks for leukocytes, actually detects enzyme leukocyte esterase, which are located in the granules of granulocytes (neutrophilic, eosinophilic and basophilic) and monocytes. Bacteria, epithelial cells and lymphocytes from the genitourinary tract do not contain esterases, thus it can’t be recognized with these test.
Neutrophil granulocytes are most commonly linked with urinary infections. In most cases, positive leukocyte esterase test normally indicates the presence of bacteria and a positive nitrite test. Infections caused by Chlamydia, Trichomonas and yeasts produce only leukocyturia without bacteriuria. The inflammation of the kidney tissues such as interstitial nephritis can produce leukocyturia, predominantly with eosinophils.
It should be known that LE test is purely indicative and should not be exclusively trusted on for definitive diagnosis, thus it can’t replace microscopic or urine culture examinations.
The urine test strip reaction for the LE detection is based on the enzymatic reaction of leukocyte esterase in catalysing the hydrolysis of an indolecarboxylic acid ester. Indoxyl product that is liberated interacts with added diazonium salt in order to produce a violet coloured azole dye, giving positive reaction result.
1) Reaction catalysed by leukocyte esterase:
Indolecarboxylic acid ester → Indoxyl + Acid
2) Acid medium:
Indoxyl + Diazonium salt → Violet azole dye
2 minutes are most commonly required for the reaction to take place.
Practical detection limit for LE test is 10-25 Leu/µl.
Can leukocyte esterase test give false positive or negative results?
A few leukocytes are normally present in urine giving a negative chemical test result. When the number of leukocytes significantly increases in the urine, this screening test will become positive. Results of this test should be considered together with a microscopic examination for leukocytes in the urine.
Strong oxidising agents or formaldehyde can give false positive results. Intense vaginal secretion may also give false positive results. False negative results are often linked with raised concentrations of protein (higher than 500 mg/dL), glucose (higher than 3 g/dL), ascorbic and oxalic acid. High specific gravity of urine may provoke leukocyte precipitation, impeding the liberation of the esterases. Hypertonic urine may also give false negative results.
The sensitivity for leukocyte esterase test
The sensitivity for leukocyte esterase with a cutoff of >10 leukocytes per mm3 ranged from 88 to 94%. While the sensitivity of leukocyte esterase and nitrite tests combination are higher than the leukocyte esterase and nitrite tests alone, it still remains too low to be used alone as a rapid urine screen.
Use of this strip in combination with another urine screen may help to decrease the number of false negative outcomes. The results achieved from combination testing may be used to “minimize” the number of urine specimens cultured and provide rapid reports of negative results.
Combur-test strips for leukocyte esterase test
Combur-test is a dry chemistry test that can be used for the early and reliable detection of kidney diseases, diabetes and urinary tract infection. It is used as a trigger for next investigations including as microscopic and bacteriological examination. It gives efficient analysis with a results coming after 60 seconds for all parameters. It can measure following parameters:
- Specific Gravity
- pH
- Leukocytes
- Nitrites
- Proteins
- Glucose
- Ketones
- Urobilinogen
- Bilirubin
- Blood
It is able to detect low concentrations of glucose and erythrocytes/hemoglobin (5 – 10 Ery/mL) in the presence of vitamin C. It can also eliminate retesting and false-negative caused by ascorbic acid (up to 400 mg/L). Combur-test strips looks like:
What may positive leukocyte esterase test indicate?
When leukocyte esterase test is positive and/or the leukocyte count in urine is high, it may indicate that there is a urinary tract or kidney infection and inflammation. The most common cause of leukocyturia is a bacterial urinary tract infection such as kidney or bladder infection.
Furthermore, to leukocytes, bacteria and erythrocytes may also be seen in the microscopic checkup. If bacteria are present, the chemical test for nitrite may also be positive.
Positive leukocyte esterase results are good indicator for present bacterial infection. Further analyses are needed for the identification of present bacteria. Positive LE results may be good a good trigger for further microscopic and bacterial examination that may diagnose following:
- Although the majority of bacteria causing infections are gram-negative bacilli, gram-positive cocci may lead to large numbers of infections in hospitalized and patients.
- coli infections most commonly cause UTI.
- Enterococci, Pseudomonas aeruginosa, and Candida spp. are mostly present in cases of catheter associated cystitis. Enterococci, which are often associated with nosocomial infections of the urinary tract, were isolated more commonly in men and have been linked with renal transplant rejection.
- Streptococcus agalactiae infections, which belong to the group B streptococci, although rare, may account for 5% of infections in pregnant female.
- In recent years, neonatal infections with group B streptococci have become more common than E. coli infections.
- Proteus mirabilis UTI can be also caused.
- Staphylococcus aureus urinary tract infections are also increasing, and their pathogenicity has been recognized. Patients at risk include: catheterized patients, males undergoing urologic procedures, those with underlying UTI pathology. Staphylococcus aureus infection may be the leading cause of renal hematogenous infection and perinephric abscesses.
- Staphylococcus saprophyticus has been also found as a urinary tract pathogen. The incidence of UTI caused by this pathogen may be even 30% in women between the ages of 16 and 25 years. There appears to be a seasonal correlation, with peaks in late summer and early fall.
- Anaerobes play a very insignificant role in UTI. But, the incidence of anaerobic bacteriuria has been reported to be 1.3% in patients with significant bacteriuria
- Although rare, pathogens such as: Chlamydia trachomatis, Ureaplasma urealyticum, Mycobacterium spp., Mycoplasma hominis, Haemophilus influenza, Legionella pneumophila, Campylobacter spp., Salmonella spp., Shigella spp., and Gardnerella vaginalis have been also related with UTI.
- Although fungi are not expected to be the cause of common urinary tract infections, they can be detected in cases of catheterization, pyelonephritis, and infections in symptomatic female patients. Fungi in urine or funguria are commonly caused by Candida albicans, Candida parapsilosis and Torulopsis (Candida) glabrata.
- Viruses and parasites are very rarely causes of UTI. However, herpes simplex virus type 2 and cytomegalovirus have been detected in patients with acute urethral syndrome with the absence of both bacteria and leukocytes. Varicella, adenovirus, herpes zoster virus, herpes simplex virus type 2 have been detected in patients with hemorrhagic cystitis.
- Trichomonas vaginalis is a protozoan linked with sexual transmission, has also been isolated from the urinary tract.
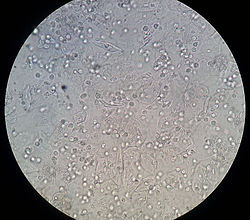
A microscopic view of a urine sediment sample from a patient suffering from urinary tract infection is shown below. Leukocytes can be seen as small round and granular.
“What can cause stuttering all of sudden? Can stuttering be cured?“