Contents
- What is methylprednisolone?
- Methylprednisolone identification
- What is the mechanism of action of methylprednisolone?
- What are the indications of methylprednisolone?
- What are the contraindications of methylprednisolone?
- What are the warnings associated with the use of methylprednisolone?
- What is the pharmacokinetics of methylprednisolone?
- What are the side effects of methylprednisolone?
- Considerations made for starting a methylprednisolone therapy
- What is the recommended dosage of methylprednisolone?
- What precautions are needed during methylprednisolone use?
- Methylprednisolone use during pregnancy and breastfeeding
- Can I take methylprednisolone with Tetanus/ diphtheria vaccine?
- Can I take methylprednisolone with ethacrynic acid/furosemide?
- Can I take methylprednisolone with anticoagulants?
- Can I take methylprednisolone with anticonvulsants?
- Can I take methylprednisolone with antidiabetic agents?
- Can I take methylprednisolone with NSAIDs?
- Can I take methylprednisolone with Grapefruit juice?
- Methylprednisolone and risk of hyperlipidemia
- Methylprednisolone and risk of fluid retention
- Methylprednisolone and risk of infections
- How long methylprednisolone stays in the system?
- Methylprednisolone and osteoporosis risk
- Methylprednisolone and tuberculin test
What is methylprednisolone?
Methylprednisolone is a drug which belongs to the class of corticosteroids and the primary purpose of the drug is to prevent the release of mediators that can cause inflammation in the body.
The drug is used for the treatment of many different inflammatory conditions such as arthritis, lupus psoriasis, allergic disorders endocrine gland disorders and those conditions which affect the skin, eyes, lungs, stomach, nervous system or blood cells.
Methylprednisolone belongs to the family of corticosteroids and more precisely these are synthetic corticosteroids. Corticosteroids normally affect the metabolism and modify the immune system in various ways.
These agents block the process of inflammation and are termed as prescription drugs. Methylprednisolone is available only on the prescription of a registered medical practitioner.
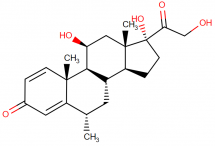
Methylprednisolone description, IUPAC name, molecular formula, weight, structure, drug class
Methylprednisolone belongs to the class of corticosteroids. It is primarily a glucocorticoid which is adrenocortical steroids and is absorbed readily from the gastrointestinal tract.
Methylprednisolone is chemically described as pregna – 1,4 – diene – 3,20-dione, 11, 17, 21-trihydroxy-6-methyl-, (6α, 11β)-.
IUPAC name: (6S,8S,9S,10R,11S,13S,14S,17R)-11,17-dihydroxy-17-(2-hydroxyacetyl)-6,10,13-trimethyl-7,8,9,11,12,14,15,16-octahydro-6H-cyclopenta[a]phenanthren-3-one
Molecular formula: C22H30O5
Molecular weight: 374.477 g/mol
Molecular structure:
Drug class: This compound belongs to the class of organic compounds known as 21-hydroxysteroids. These are steroids carrying a hydroxyl group at the 21-position of the steroid backbone.
Methylprednisolone identification
Methylprednisolone is usually white to practically white in color and exists in the form of crystalline powder. It is odorless and is practically insoluble in water.
It is only slightly soluble in acetone and chloroform and sparingly soluble in alcohol, dioxane and in methanol while being very slightly soluble in ether.
What is the mechanism of action of methylprednisolone?
Methylprednisolone belongs to the class of corticosteroids and this drug is specifically a glucocorticoid.
Glucocorticoids have a high affinity for the specific cytoplasmic receptors and bind with them after crossing the cell surface membranes thereby modifying the process of transcription and protein synthesis.
Due to this effect, glucocorticoids can inhibit the process of leukocyte infiltration at the site of inflammation and also interfere with the mediators responsible for inflammatory response and hence suppress the humoral immune responses.
These corticosteroids which are responsible for the anti-inflammatory response are thought to involve lipocortins which are phospholipase A2 inhibitory proteins and control the biosynthesis of prostaglandins and leukotrienes which are the potent mediators of inflammation.
Glucocorticoids can also supress the inflammatory process by numerous other pathways. They enter the target tissues and bind with specific intracellular receptor proteins thereby altering the expression of corticosteroid responsive genes.
The glucocorticoid specific receptors which are present in the cytoplasm of the cell bind with the steroid ligands and result in the formation of hormone-receptor complexes which are eventually translocated to the nucleus of the cell.
In the nucleus, these hormone-receptor complexes bind with the specific DNA sequences and alter their expression.
These complexes can also cause the synthesis of new proteins by inducing the transcription of mRNA.
These newly synthesized proteins includelipocortin which is a potent inhibitor of phospholipase A2a which result in the blockage of the synthesis of prostaglandins, leukotrienes, and platelet activating factor.
When these inflammatory mediators are not synthesized so the process of inflammation is stopped.
Glucocorticoids also have the ability to block cyclooxygenases, cytokines, interleukins, and adhesion molecules which are arachidonic acid metabolites and also enzymes such as collagenases, all of which are other mediators of inflammation.
What are the indications of methylprednisolone?
Methylprednisolone is a glucocorticoid belonging to the class of synthetic corticosteroids and is indicated in a variety of conditions which are stated as:
Endocrine disorders:
These include:
- Primary or secondary adrenocortical insufficiency
- Congenital adrenal hyperplasia
- Nonsuppurative thyroiditis
- Hypercalcemia associated with cancer
Rheumatic disorders:
For the short-term administration, as adjunct therapy in order to help patients to cope with an acute episode or exacerbation in:
- Rheumatoid arthritis which also includes juvenile rheumatoid arthritis
- Ankylosing spondylitis
- Acute and subacute bursitis
- Synovitis of osteoarthritis
- Acute nonspecific tenosynovitis
- Post traumatic osteoarthritis
- Psoriatic arthritis
- Epicondylitis
- Cute gouty arthritis
Collagen diseases:
In selected cases in case of an exacerbation or as maintenance therapy in:
- Systemic lupus erythematosus
- Systemic dermatomyositis
- Acute rheumatic carditis
Dermatological diseases:
These include:
- Bullous dermatitis herpetiformis
- Severe erythema multiforme
- Severe seborrheic dermatitis
- Exfoliative dermatitis
- Mycosis fungoides
- Pemphigus
- Severe psoriasis
Allergic states:
When conventional treatment is incapable to control severe or progressing allergic reaction then the drug can be used in:
- Seasonal or perennial allergic rhinitis
- Drug hypersensitivity reactions
- Serum sickness
- Contact dermatitis
- Bronchial asthma
- Atopic dermatitis
Ophthalmic diseases:
In the treatment of severe acute and chronic inflammatory or allergic processes which involve the eye:
- Allergic corneal marginal ulcers
- Herpes zoster ophthalmicus
- Anterior segment inflammation
- Sympathetic ophthalmia
- Keratitis
- Optic neuritis
- Allergic conjunctivitis
- Chorioretinitis
- Iritis and iridocyclitis
Respiratory diseases:
These include:
- Symptomatic sarcoidosis
- Berylliosis
- Loeffler’s syndrome which can not be managed by other means
- Fulminating or disseminated pulmonary tuberculosis
- Aspiration pneumonitis
Hematologic disorders:
These include:
- Idiopathic thrombocytopenic purpura in adults
- Secondary thrombocytopenia in adults
- Autoimmune hemolytic anemia
- Erythroblastopenia
- Congenital hypoplasticanemia
Neoplastic diseases:
For the palliative management of:
- Leukemias and lymphomas in adults
- Acute leukemia of childhood
Gastrointestinal diseases:
To provide relief to the patients during the critical period of the following diseases:
- Ulcerative colitis
- Regional enteritis
Miscellaneous disorders:
- It can be used for the remission of proteinuria or for the induction of diuresis in patients with nephrotic syndrome, without uremia, which could be due to lupus erythematosus or which could be of the idiopathic type.
- For the treatment of acute exacerbations of multiple sclerosis
- Trichinosis with neurologic or myocardial involvement
- The use of appropriate antituberculous chemotherapy in combination with tuberculous meningitis with subarachnoid block or impending block.
What are the contraindications of methylprednisolone?
Methylprednisolone is a synthetic glucocorticoid and is contraindicated in individuals who are allergic to corticosteroids or any of the steroidal analogs. Moreover, the drug is also contraindicated in patients having conditions such as:
- Serious untreated infections
- Systemic fungal infection
- Premature infants as the formulations contain benzyl alcohol
- Traumatic brain injury
- Patients receiving immunosuppressive doses of corticosteroids are contraindicated to be administered live, or live, attenuated vaccines.
Apart from this, intrathecal administration of methylprednisolone is contraindicated as well as intramuscular administration is also contraindicated in patients with idiopathic thrombocytopenic purpura.
What are the warnings associated with the use of methylprednisolone?
Corticosteroids have the ability to mask the signs of an infection while new infections can occur during their use.
These infections may be caused by any type of pathogen including viral, fungal, protozoan or helminthic infection in any part of the body.
These infections may be associated with the use of corticosteroids, either alone or in combination with immunosuppressive agents which affect various types of immunities including cellular immunity, humoral immunity or normal functioning of the neutrophils.
These infections vary from mild to severe while may be fatal at times. These complications increase on increasing the dose of corticosteroids and even result in decreased resistance and an inability to localize the infection with their use.
Those patients who suffer from unusual stress during therapy with corticosteroids are indicated to use an increased dose of rapidly acting corticosteroid before, during and after a stressful situation.
Using corticosteroids for a longer period of time may result in posterior subcapsular cataracts while also causing glaucoma with the possibility of damaging the optic nerve and may also enhance the establishment of secondary ocular infections caused by fungi or viruses.
Live or live, attenuated vaccines are contraindicated to be administered to the patients already receiving immunosuppressive doses of corticosteroids.
Such patients may be given killed or inactivated vaccines, however, there might be a diminished response to such vaccines.
All corticosteroids cause an increase in the excretion of calcium while they might also cause an elevation of blood pressure, salt, and water retention and may also cause an increased excretion of potassium.
These patients should be recommended to restrict their dietary salt intake as well as use potassium supplements.
These agents suppress the immune system and hence making individuals more susceptible to infections. If such individuals get infected with chicken pox or measles then they can experience a very severe or even a fatal course of the infection.
In such cases, care should be taken to avoid exposure to such pathogens. Similarly, those patients who are having known or suspected strongyloides infestation should be treated with corticosteroids with great care as in such patients, corticosteroid induced immunosuppression may cause strongyloides hyper infection.
What is the pharmacokinetics of methylprednisolone?
Methylprednisolone is usually administered via the oral route. The formulations that are available for parnteral route include methylprednisolone sodium succinate and methylprednisolone acetate suspension.
Succinate preparation is used for IV and IM route whereas acetate suspension can be injected IM, intraarticular, intralesional or direct into soft tissue injection.
As soon as methylprednisolone reaches the blood on the body it shows a rapid distribution into kidneys, skin tissues, liver, muscles, and intestines. It has also been detected in the breast milk as well as has shown penetration in the blood brain barrier.
The drug is metabolized in the liver through a number of mechanisms to inactive metabolic products.
Along with these inactive metabolites, a minute quantity of unchanged drug is together excreted in urine. Methylprednisolone shows an elimination half life of 18 – 36hours.
Oral route:
Following an oral dose, methylprednisolone shows a rapid absorption and thus a high bioavailability. Peak plasma concentrations are obtained within 1 to 2 hours.
Intravenous route:
When methyl prednisolone sodium succinate is given to the patient via IV route, the onset of action is after 1 hour of administration and complete excretion is seen within 12 hours post injection. A repeated equal dose is required almost every 4 to 6 hours when continuous high plasma levels are needed in treatment.
Intramuscular route:
Soon after methylprednisolone sodium succinate is administered via IM route, a rapid systemic absorption is seen.
Other routes:
When methylprednisolone sodium succinate is administered in the joints via intra-articular injection, the absorption of the drug is extremely slow. It may take upto 7 days for the drug to completely absorb.
What are the side effects of methylprednisolone?
The drug may cause common to serious side effects. Many of these effects may be eliminated by the discontinuation of the drug. Following are some of the serious side effects which might need immediate medical attention, caused by methylprednisolone:
Fluid and electrolyte disturbances:
- Sodium retention
- Congestive heart failure in susceptible patients
- Hypertension
- Fluid retention
- Potassium loss
- Hypokalemic alkalosis
Musculoskeletal:
- Muscle weakness
- Loss of muscle mass
- Steroid myopathy
- Osteoporosis
- Tendon rupture, particularly of the Achilles tendon
- Vertebral compression fractures
- Aseptic necrosis of the femoral and humeral heads
- Pathologic fracture of the long bones
Gastrointestinal:
- Peptic ulcer with possible perforation and hemorrhage
- Pancreatitis
- Abdominal distention
- Ulcerative esophagitis
- Corticosteroid treatment can also lead to an increase in alanine transferase, aspartate transaminase, and alkaline phosphatase.
Dermatologic:
- Impaired wound healing
- Petechiae and ecchymoses
- Have the ability to suppress reactions to skin tests
- Thin fragile skin
- Facial erythema
- Increased sweating
Neurological:
- Convulsions
- Vertigo
- A headache
- Increased intracranial pressure with papilledema usually after treatment
Endocrine:
- Development of cushingoid state
- Suppression of growth in children
- Menstrual irregularities
- Decreased carbohydrate intolerance
- Manifestations of latent diabetes mellitus
- Increased requirements of insulin or oral hypoglycemic agents in diabetes
- In times of stress such as in trauma, surgery or illness may lead to secondary adrenocortical and pituitary unresponsiveness
Ophthalmic:
- Posterior subcapsular cataracts
- Increased intraocular pressure
- Glaucoma
- Exophthalmos
Metabolic:
- Negative nitrogen balance due to protein catabolism
In addition to these effects, the drug may also cause some common side effects including:
- Headache
- Nausea and vomiting
- Weight gain
- Confusion, excitement, and restlessness
- Swelling of your ankles, feet or hands
- Skin problems such as acne, thin skin, and shiny skin
- Increased thirst
- Infection
- High blood pressure
- Depression
- Facial flushing
- Insomnia
- Irritability
- Mild stomach pain or bloating
Considerations made for starting a methylprednisolone therapy
Putting a patient on steroids is the last option that should be utilized. This is possibly due to the reason of a number of side effects that occur with the use of steroids. The possibility of facing these unfortunate effects can occur by taking a single dose, during the treatment period or even days after the therapy has been stopped. In order to avoid these to take place, certain considerations are to be made which are listed as below:
- The prescriber should have a strong knowledge of the indication for which methylprednisolone is prescribed.
- The shortest duration of therapy should be selected for example the best time period is between 5 – 7 days. A prolonged course has a greater probability of side effects to occur.
- The patient who is on treatment with methylprednisolone should be monitored at regular intervals and all these measurements should be recorded.
- It is recommended to prescribe methylprednisolone (or any steroid) either in a single dose or divided doses to be administered in the first half of the day. This is done to avoid any trouble in the normal sleep cycle.
- In addition to methylprednisolone, it is always better to prescribe a prophylactic agent that helps to protect the gastric lining.
- For this purpose, proton pump inhibitors are prescribed to even those individuals who have no past medical history of peptic ulcer disease.
- When the therapy with methylprednisolone is done by keeping normal dose for a longer time or higher doses for a shorter time, the risk of developing a yeast infection on skin increases.
- In such cases, an anti-fungal agent mostly Nystatin (100000 units) or 1ml four times a day is prescribed prophylactically.
What is the recommended dosage of methylprednisolone?
The dosage decided should be individualized on the basis of the indication for which is it being prescribed and the response of the patient towards the therapy.
Allergic rhinitis
A dose of 80 – 120 mg IM helps to overcome the symptoms
Alopecia and other dermatological diseases
- Oral route:
The first dose can be a maximum of 4 – 48mg which can be administered at a single time or in divided doses. Once maintained and an acceptable response is obtained, the dose is then gradually tapered at proper intervals until the lowest dose with an adequate clinical response is obtained.
Day 1: 24mg Day 2: 20mg Day 3: 16mg Day 4: 12mg Day 5: 8mg Day 6: 4mg
- Parenteral route:
The starting dose can be in between 40 to 120mg IM given once a week for 1 to 4 weeks.
For acute dermatitis – relief can be obtained within 8 -12 hours
For chronic dermatitis – relief can be obtained within 10 days
- Intralesional administration:
This route is used lessen the occurrence of dermal and subdermal atrophy.
First dose: 20 – 60mg injected directly into the lesion.
In larger lesions: 2-4 injections of 20 – 40mg.
Rheumatoid arthritis
- Oral route:
The first dose can be a maximum of 4 – 48mg which can be administered at a single time or in divided doses. Once maintained and an acceptable response is obtained, the dose is then gradually tapered at proper intervals until the lowest dose with an adequate clinical response is obtained.
Day 1: 24mg Day 2: 20mg Day 3: 16mg Day 4: 12mg Day 5: 8mg Day 6: 4mg
- Parenteral route:
The dose can be in between 40 to 120mg IM given once a week.
Note: corticosteroids are not able to suppress the adrenocorticoid activity to an adequate level when they are at the time of maximal activity which is in between 2 am to 8 am.
When the treatment with methylprednisolone is required for chronic periods, it is suggested to choose alternate days for the administration of the drug.
- Intraarticular injection
Dose varies according to the severity of the doses.
In large joint (for example knee, shoulder, and ankles) 20mg -80mg
In medium joints (like elbow and wrist) 10mg – 40mg
In small joints (for example metacarpophalangeal, interphalangeal and sternoclavicular) 4mg – 10mg.
On the basis on which the patients get relief, these injections can be administered every 1 – 5 weeks.
Adrenogential syndrome
Loading dose: 40mg IM every 2nd week.
Maintenance dose can be decided as per the needs of the individual patient.
Anti-inflammatory
- Oral route:
The first dose can be a maximum of 4 – 48mg which can be administered at a single time or in divided doses.
Once maintained and an acceptable response is obtained, the dose is then gradually tapered at proper intervals until the lowest dose with an adequate clinical response is obtained.
Day 1: 24mg Day 2: 20mg Day 3: 16mg Day 4: 12mg Day 5: 8mg Day 6: 4mg
- Parenteral route:
Sodium succinate formulation can be given via IV and IM (the emergency route is IV)
30mg/ kg over a minimum times period of 30 minutes repeated every 4 to 6 hours.
Acetate suspension formulation (IM only)
First dose: 4 -120mg IM (if relief is not obtained from the first dose then additional injections can be given.
Maintenance dose: once the patient is stabilized and an acceptable response is obtained, the dose is then gradually tapered at proper intervals until the lowest dose with an adequate clinical response is obtained.
Asthma
- Oral route:
Burst therapy involves the administration of 32-64mg orally once or in divided doses.
- Parenteral route:
Sodium succinate formulation can be given via IV and IM (the emergency route is IV) 30mg/ kg over a minimum times period of 30 minutes repeated every 4 to 6 hours.
What precautions are needed during methylprednisolone use?
You should always tell your doctor or pharmacist if you are allergic to methylprednisolone or any other corticosteroids or if you are allergic to benzyl alcohol.
Moreover, you should also tell him about any other prescription or non-prescription medicines, vitamins, nutritional supplements or any herbal products that you are using currently or have used in the past.
You should also tell your doctor if u have any fungal infection or if you have idiopathic thrombocytopenic purpura so in such cases your doctor will not prescribe you methylprednisolone.
You should also tell him if you have ever had tuberculosis, cataracts, Cushing’s syndrome, high blood pressure, heart failure, myasthenia gravis, any mental illness, seizures, ulcer, liver, kidney or thyroid disease.
In case you are pregnant or are planning to get pregnant or breastfeeding then you should inform this to your doctor accordingly so that he can adjust the medication accordingly.
If you are having any surgery which could also include a dental surgery, so you should tell your doctor beforehand that you are using methylprednisolone and you should not have any vaccinations while using the drug.
It is the duty of your doctor to tell you that while using this medication, your ability to fight infections reduces markedly.
In such cases, it is recommended to stay away from sick people and especially those who already have cowpox or measles. In case of any problem, you should talk to your doctor immediately and seek medical attention.
Methylprednisolone use during pregnancy and breastfeeding
Methylprednisolone is included in pregnancy category C by the US FDA. This implies that the drug should be used with caution during pregnancy and should only be prescribed if the benefits of the drug are more than the risks.
There is not enough evidence of the safety of the drug in pregnant women because of the lack of well-controlled studies but still should be used with caution in pregnancy.
The drug should be used with caution by mothers who are breastfeeding the new-borns. There is evidence that the drug is excreted into breast milk but in low amounts.
However, the drug should only be used by such mothers if the benefits outweigh the risks. The drug usually does not cause any significant effects in new-borns at normal doses but can cause serious effects if taken in large amounts by the mother.
Can I take methylprednisolone with Tetanus/ diphtheria vaccine?
Corticosteroids are accountable for depressing the immune system within the body. As methylprednisolone is a corticosteroid it will suppress the immunological response that is evoked when vaccination is given.
When tetanus/ diphtheria vaccine is administered to the patient who is already using methylprednisolone, a low response against the vaccine is produced which is not sufficient.
This, in turn, will make the patient more prone to suffer from infection. In such cases, it is advised to administer the vaccine either 2 weeks before the use of methylprednisolone or 2 weeks after the corticosteroid therapy is stopped.
Can I take methylprednisolone with ethacrynic acid/furosemide?
Methylprednisolone is been responsible for bringing out the electrolyte imbalance in the body. This is done by likely retention of water and salt.
Loop diuretics including ethacrynic acid and furosemide work by preventing the reabsorption of water and ions from the descending limb.
When corticosteroids are administered in patients who are using diuretics, it will oppose their action and reduce the diuretic efficacy. As a result, chances for hypokalemia increases.
Can I take methylprednisolone with anticoagulants?
Patients are commonly prescribed corticosteroids for the treatment of certain inflammatory disorders or diseases which involve the immune system.
Several of these patients are also given anticoagulants for the blood thinning purpose. When both of these drugs are coadministered it has been observed that methylprednisolone increases the anticoagulant outcome of warfarin and as result the possibility of GI bleeding increases.
In such patients, it is recommended to closely monitor INR. Usually, on the coadministration of these drugs, the international normalized ratio (INR) is increased.
Can I take methylprednisolone with anticonvulsants?
Phenytoin, carbamazepine, and phenobarbital are mostly used medicines for the treatment of convulsions.
When a patient who is being given corticosteroids has to be given any of the anticonvulsants, it has been observed these drugs promotes the metabolism of methylprednisolone.
As a result, the efficacy of methylprednisolone is reduced significantly.
Due to this effect, larger doses of methylprednisolone are required which is not safe to be used as declared by FDA.
When dosage modifications are to be made for methylprednisolone, close monitoring of vitals and other signs should be checked.
This effect of anticonvulsants on the metabolism of methylprednisolone lasts long even the medications have been discontinued.
Can I take methylprednisolone with antidiabetic agents?
A number of classes of drugs are used for the control of blood glucose levels. Each class exerts its action in a different way to lower the blood glucose levels.
Corticosteroids when given increase the blood glucose level and this effect is more dominant than any of the effect of the anti-diabetic agent.
Due to this antagonist effect, corticosteroids lead to hyperglycemia. It is important to check the blood glucose levels at a more frequent rate when the treatment with both drug classes is made.
Can I take methylprednisolone with NSAIDs?
This class includes drugs which are used for their anti-inflammatory, antipyretic and analgesic action but are nonsteroidal in nature. They function by interfering with the prostaglandins produced in the stomach.
This, in turn, causes reduced mucosal blood flow and mucus secretion exposing off the mucosal lining to erode by the action of the acid. In a similar way, methylprednisolone acts on the prostaglandins and reduces the protective layer form the stomach.
When both the NSAIDs are used in combination with methylprednisolone this exposure of the musical lining is done more quickly increasing the risk of ulcers in the stomach.
For the treatment of drug-induced ulcers, proton pump inhibitors are usually the first line of therapy.
Can I take methylprednisolone with Grapefruit juice?
Grapefruit juice may increase the plasma concentrations of orally administered drugs that are substrates of the CYP450 3A4 isoenzyme such as methylprednisolone.
However, the interaction seems to affect primarily those drugs that undergo significant presystemic metabolism by CYP450 3A4 (i.e., drugs with low oral bioavailability), presumably due to the fact that grapefruit juice inhibits primarily intestinal rather than hepatic CYP450 3A4.
Because pharmacokinetic interactions involving grapefruit juice are often subject to a high degree of interpatient variability, the extent to which a given patient may be affected is difficult to predict.
Methylprednisolone and risk of hyperlipidemia
Corticosteroids such as methylprednisolone may elevate serum triglyceride and LDL cholesterol levels if used for longer than brief periods.
Patients with preexisting hyperlipidemia may require closer monitoring during prolonged corticosteroid therapy, and adjustments made accordingly in their lipid-lowering regimen.
Methylprednisolone and risk of fluid retention
Corticosteroids such as methylprednisolone may cause hypernatremia, hypokalemia, fluid retention, and elevation in blood pressure.
These mineralocorticoid effects are most significant with fludrocortisone, followed by hydrocortisone and cortisone, then by prednisone and prednisolone.
The remaining corticosteroids, betamethasone, dexamethasone, methylprednisolone, and triamcinolone, have little mineralocorticoid activities.
However, large doses of any corticosteroid can demonstrate these effects, particularly if given for longer than brief periods.
Therapy with corticosteroids should be administered cautiously in patients with preexisting fluid retention, hypertension, congestive heart failure, and/or renal dysfunction. Dietary sodium restriction and potassium supplementation may be advisable.
Methylprednisolone and risk of infections
The immunosuppressant and anti-inflammatory effects of corticosteroids, particularly in higher dosages, may decrease host resistance to infectious agents, decrease the ability to localize infections, and mask the symptoms of infection. Secondary infections may be more likely to develop.
In general, corticosteroids should not be used in patients with active infections, especially systemic fungal infections, unless they are medically necessary and effective antimicrobial therapy or other appropriate treatment has been instituted.
However, for corticosteroid-dependent patients who develop a severe or life-threatening infection, continuation of corticosteroid therapy with at least physiologic replacement dosages should be considered, since these patients may have secondary adrenocortical insufficiency. Removal of external steroid during periods of stress may be detrimental to these patients.
How long methylprednisolone stays in the system?
The half-life for all formats of methylprednisolone (immediate-release and delayed-release) ranges from 2 to 3 hours after conversion to “prednisolone.” This means that in approximately 3 hours, 50% of the dose you ingested will have been cleared from systemic circulation.
If considering the 2 to 3 hour documented half-life, the methylprednisolone should theoretically be cleared from your system between 11 and 16.5 hours post-ingestion.
Some sources suggest that the half-life of pharmacologically active “prednisolone” may be slightly longer than 2 to 3 hours.
One source suggests that its half-life could be 2 to 4 hours with an average of ~3.6 hours. This would indicate that elimination of prednisolone concentrations from systemic circulation would take just under 20 hours.
In other words, both methylprednisolone and prednisolone should be cleared from your body within a 24 hour period after stopping.
However, just because you no longer have prednisone circulating throughout your bloodstream certainly doesn’t mean you should be feeling 100% better.
Prednisolone facilitates numerous physiological alterations throughout your body that could linger for a long-term following discontinuation
Methylprednisolone and osteoporosis risk
Corticosteroids such as methylprednisolone reduce osteoblastic function and inhibit the absorption of intestinal calcium, which can result in bone resorption and bone loss during prolonged therapy.
In addition, bone matrix may be affected by the protein-catabolic effects of corticosteroids, especially when given in high dosages or for prolonged periods, leading to aseptic necrosis and fractures.
Long-term or high-dose corticosteroid therapy should be administered cautiously and only if necessary in patients with or at risk for osteoporosis. Adverse skeletal effects may be minimized by alternate-day or intermittent administration.
Any patient receiving prolonged therapy with the equivalent of 7.5 mg prednisone/day or more are at risk for glucocorticoid-induced osteoporosis and should be managed according to The American College of Rheumatology (ACR) guidelines.
Methylprednisolone and tuberculin test
In patients with latent tuberculosis or tuberculin reactivity, the use of pharmacologic dosages of corticosteroids including methylprednisolone may cause a reactivation of the disease.
Close monitoring for signs and symptoms of tuberculosis is recommended if corticosteroid therapy is administered to patients with a history of tuberculosis or tuberculin reactivity. During prolonged corticosteroid therapy, tuberculosis chemoprophylaxis may be considered.